Journal:Health informatics: Engaging modern healthcare units: A brief overview
| Full article title | Health informatics: Engaging modern healthcare units: A brief overview |
|---|---|
| Journal | Frontiers in Public Health |
| Author(s) | Yogesh, M.J.; Karthikeyan, J. |
| Author affiliation(s) | Vellore Institute of Technology |
| Primary contact | Email: yogeshmj dot nie at gmail dot com |
| Year published | 2022 |
| Volume and issue | 10 |
| Article # | 854688 |
| DOI | 10.3389/fpubh.2022.854688 |
| ISSN | 2296-2565 |
| Distribution license | Creative Commons Attribution 4.0 International |
| Website | https://www.frontiersin.org/articles/10.3389/fpubh.2022.854688/full |
| Download | https://www.frontiersin.org/articles/10.3389/fpubh.2022.854688/pdf (PDF) |
Abstract
With a large amount of unstructured data finding its way into health systems, health informatics implementations are currently gaining traction, allowing healthcare units to leverage and make meaningful insights for doctors and decision makers using relevant information to scale operations and predict the future view of treatments via information systems communication. Now, around the world, massive amounts of data are being collected and analyzed for better patient diagnosis and treatment, improving public health systems and assisting government agencies in designing and implementing public health policies, while also instilling confidence in future generations who want to use better public health systems.
This article provides an overview of the Health Level 7 FHIR architecture, including the workflow state, linkages, and various informatics approaches used in healthcare units. The article also discusses future trends and directions in health informatics and its successful application to benefiting public health safety. With the advancement of health informatics technologies, however, healthcare units face new issues that must be addressed with appropriate adoption policies and standards.
Keywords: health informatics, public health, information systems, health policy, public health systems
Introduction
Machine learning is the fastest-growing topic in computer science today, and with it a health informatics implementation of ML is one of the more difficult problems to solve.[1][2]
Emerging economies are increasing their investments in healthcare, which makes sense and encourages health professionals to adopt sound frameworks and regulatory standards, as well as health IT, to improve the quality and efficacy of care.[3] In this expanding field, new age occupations can be established. This new field has the potential to be a lucrative career path in the future. With a clear flow of information across many medical subsystems, adoption of electronic health record systems (EHRs) will improve the health care system going forward.[4]
Big data is frequently employed in the field of health informatics, as new data is constantly pouring into the system, requiring analysis and interpretation in order to make rational decisions.[5][6] This big data has ushered in a new era for healthcare companies to improve decision-making through the comprehensive integration of data from a range of sources, allowing for much faster and more effective decision making.[7] As such, within and outside of the medical industry, computational health informatics has become an emerging field of study.[7][8][9]
In recent years, the healthcare industry has seen a rapid growth in medical and healthcare data, which can be used to improve facilities and public healthcare utilization and implementation using novel treatment and diagnosis methodologies. In turn, this more efficient use of healthcare data gives patients confidence in using the best public healthcare services available and aids governments in developing better healthcare policies.[10]
In today's increasingly complex social and economic environment, at hand is the vital issue of improving quality of offered healthcare services while lowering prices. This is largely what health informatics has attempted to solve. The major purpose of health informatics is to increase our understanding of medicine and medical practice by using real-world medical data. In the scope of healthcare, health informatics is practically a blend of information science and computer science.[11]
At the core of health informatics has historically been a collection of computerized systems for assisting patient analysis and diagnosis. More recent technologies have emerged that make it even easier for clinicians to make better healthcare decisions.[12][13] As health informatics continues to evolve, it promises to improve public health activities through the advanced application of information and communication technologies (ICT).[14] ICTs have been shown to help healthcare systems increase productivity, which has resulted in significant cost savings in operations and service delivery. For administrative and healthcare objectives, ICTs have already proven to be quite effective. Additionally, new prospects for new medical equipment and systems are opening up as ICTs become smaller, quicker, wireless, and remotely controlled.
The internet and web have recently brought up new possibilities for increasing the response time of healthcare services, while also lowering costs. It is clear that we are in the early stages of a new era that will fundamentally alter the way healthcare services are provided. This will help us acquire the public's trust in using high-quality healthcare services. However, new e-Health services and technology must still be researched, developed, promoted, and disseminated with significant effort. With the COVID-19 pandemic presently sweeping the globe, increasing ICT use has demonstrated that healthcare can and will become more contactless in the future, with fresh means of treating patients and providing healthcare services emerging. This is a popular yet difficult research subject since it necessitates interdisciplinary competence.[15]
Additionally, as big data continues to increasingly find its way into healthcare, additional challenges exist in the effective use of big data within ICT frameworks. For example, big data in healthcare is intimidating not only because of its sheer magnitude, but also due to the variety of data types and the pace with which it must be managed. To gain people' trust and give quality healthcare services, all health service providers are now putting in extra effort to use the most up-to-date technologies to effectively use big data to provide quality health services and advanced treatments.
Various requirements drive innovation in this industry, such as finding appropriate accommodation with standardization and coordinating the acquisition and implementation of newer healthcare systems and services on a national/international level. With COVID-19 still threatening disruption in the healthcare sector, investments in this sector are gaining steam with new-age healthcare units in many nations, and growing economies such as India and China will continue to play a vital role in providing quality healthcare services to its citizens in the future. At the same time, those new-age healthcare units and systems will aid in dramatically lowering costs, making public healthcare systems more dependable, and instilling citizens' confidence in using inexpensive, high-quality healthcare.
Related work
"Big data" is a term used to describe a significant volume of data that is collected and stored yet has outgrown standard data management and analysis solutions. Solutions like Hadoop and Spark, according to Roger Fyre and Mark McKenney, have arisen to solve some of these big data concerns.[16] For example, researchers have used Hadoop to implement a variety of parallel processing algorithms to efficiently handle geographical data.[17][18] Multistage map and reduce algorithms, which generate on-demand indexes and retain persistent indexes, are the end result of these techniques.[19]
Other techniques such as predictive analytics and data mining have also been employed. Much of the current work on predictive analytics, particularly in clinical contexts, is aimed at improving health and financial outcomes, which will aid in making better decisions.[20] Data mining, which is defined as the processing and modeling of huge amounts of medical/health data to identify previously unknown patterns or associations, is another important machine learning approach.[21][22] Data mining has been used, for example, in the collection of data for diseases such as cancer and neurological disorders in order to improve disease prognosis.[23][24] Cancer detection and diagnosis, as well as other health-related issues, have been made possible because to these breakthroughs.[25] Machine learning is also crucial in the testing and development of various models that take into account clinical and other important medical characteristics for decision making.
Deep learning is now also being used to solve more difficult problems in the arena of health informatics.[26][27] For example, advances in medical imaging and its data management have made positive contributions to decision making. Today, medical imaging incorporates capabilities such as image segmentation, image registration, annotation, and database retrieval, holding greater promise for decision makers. As such, new deep learning and machine learning models can be employed with medical imaging for speedier decision making.[26] However, this means researchers in the fields of data science, machine learning, and deep learning remain in high demand for developing effective algorithms that adapt to changing data.
Holzinger et al.[28] examined many approaches to developing an explainable prediction model for the medical domain. Prediction explanations can be useful in a variety of situations, including teaching, learning, research, and even the courtroom. Similarly, the demand for interpretable and explainable models is growing in the medical field. However, these models must be able to re-enact the decision-making and knowledge-extraction processes. Ribeiro et al.[29] have emphasized this requirement, discussing how machine learning models are essentially black boxes. Understanding the reasons for predictions can help to build trust, better assess model performance, and construct better, more accurate, and correct models by providing insights into the model. They propose the LIME algorithm[29] for explaining predictions of any model. Similarly, though dealing with neural machine translation, the proposed model of Bahdanau et al.[30] can be used in a variety of other applications such as healthcare.
Introduction to HL7 FHIR architecture
In the last two decades, EHRs have been widely implemented in the United States to improve healthcare quality, increase patient happiness, and reduce healthcare costs.[31][32][33] As growing countries such as India, China, and Bangladesh experiment with innovative ways to establish EHR systems, they will significantly aid in the development of effective public health systems in those countries. In all cases, at the core of most effective EHRs is Health Level 7's (HL7's) Fast Health Interoperability Resources (FHIR) architecture.
The basic idea behind HL7's FHIR (pronounced “fire”) was to create a set of resources and then create HTTP-based REST application programming interfaces (APIs) to access and use these resources. FHIR uses components called "resources" to access and perform operations on patient's health data at the granular level. This feature distinguishes FHIR from all other standards because it was not present in any earlier version of HL7 (v2, v3) or the HL7 clinical document architecture (CDA).[34]
The fundamental building blocks of FHIR are the so-called resources, which are generic definitions of common health care categories (e.g., patient, observation, practitioner, device, condition). For data interchange and resource serialization, FHIR employs JavaScript object syntax and XML structures. FHIR not only supports RESTful resource exchange but also manages and documents an interoperability paradigm.
FHIR has grown in popularity and is being increasingly used by the healthcare industry since its inception. In 2018, six major technology companies—including Microsoft, IBM, Amazon, and Google—vowed to remove barriers to healthcare interoperability and signed a statement mentioning FHIR as an emerging standard for the interchange of health data. With the incorporation of Substitutable Medical Applications Reusable Technologies (SMART), a platform for interoperable applications[35], FHIR can be expected to attract even more attention to digital health tools in the future. As is, the use of FHIR for medical data transmission has the potential to deliver benefits in a wide range of disciplines, including mobile health apps, EHRs, precision medicine, wearable devices, big data analytics, and clinical decision support.
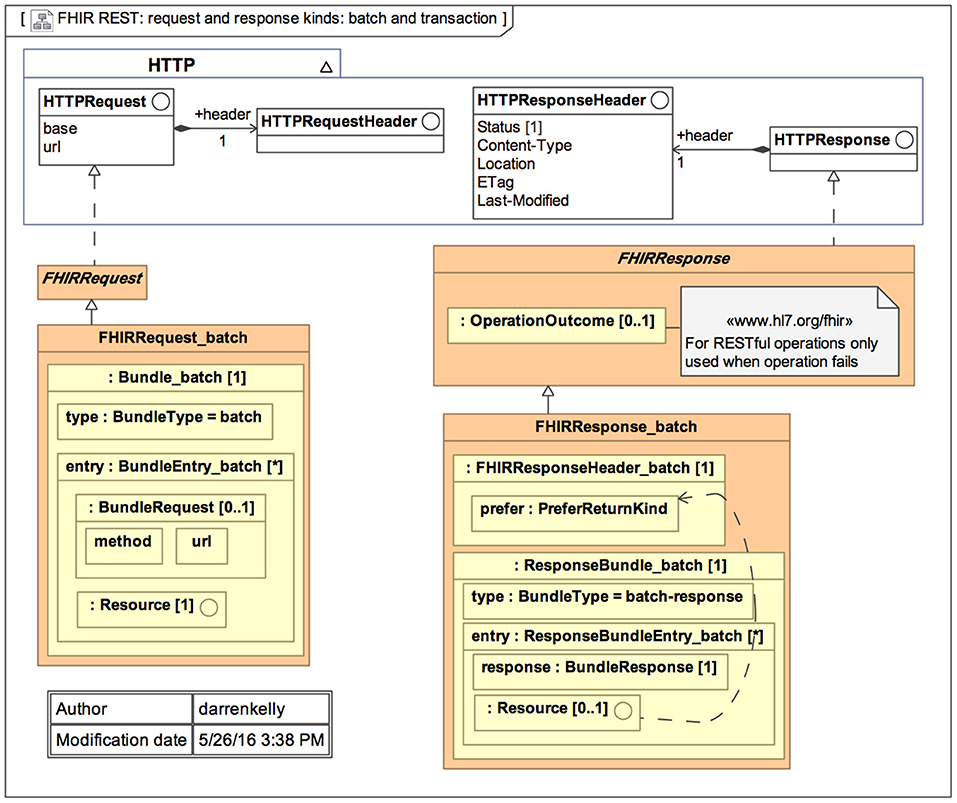
The primary goal of FHIR is to reduce implementation complexity while maintaining information integrity. Furthermore, this new standard integrates the benefits of existing HL7 standards (v2, v3, and CDA) and is projected to overcome their drawbacks. FHIR enables developers to create standardized browser applications that allow users to access clinical data from any healthcare system, regardless of the operating systems and devices used. Figure 1 represents the general architecture of FHIR.[34]
|
FHIR for patient access to medical records
FHIR is an HL7 standard for electronically transferring healthcare information. The Centers for Medicare and Medicaid Services (CMS) Interoperability and Patient Access final regulation, announced in 2020, mandates all CMS-regulated payers to use FHIR version 4. Unlike earlier releases, the fourth iteration is backward compatible, ensuring that software suppliers' solutions will not become obsolete when a new FHIR version is released.
The FHIR standard defines a collection of HTTP-based RESTful APIs that allow healthcare platforms to exchange and share data in XML or JSON format. FHIR offers mobile apps, which users can obtain from the Apple App Store or Google Play in order to access their medical records and claims data.
FHIR's basic exchangeable data piece is known as a resource. Each resource is formatted similarly and contains roughly the same amount of data. Each resource offers information about patient demographics, diagnosis, prescriptions, allergies, care plans, family history, claims, and so on, depending on the kind. They span the complete healthcare workflow and can be used independently or as part of a larger document.
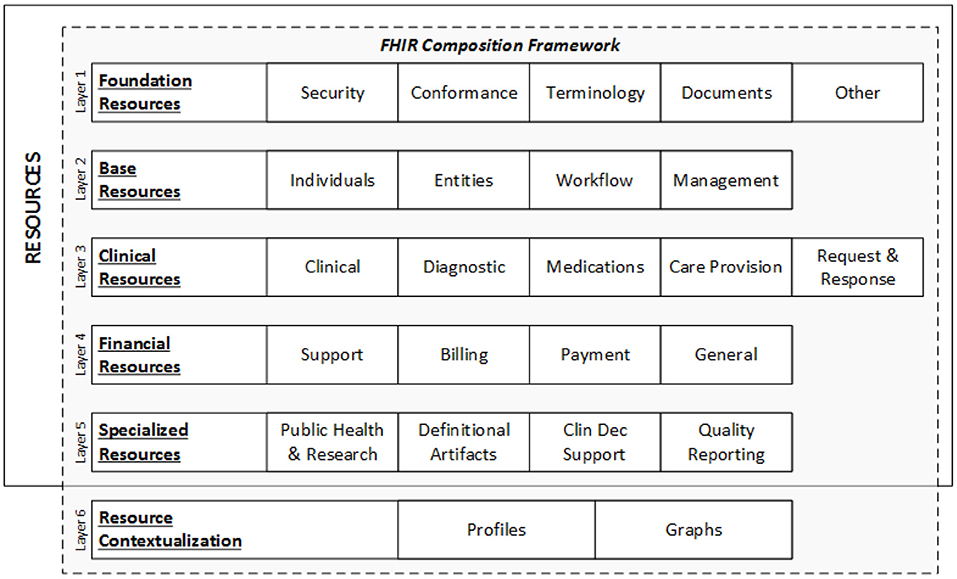
Each resource is given a unique ID, and many health systems, insurers, patients, and software developers can access the underlying data element using an API. Figure 2 represents the data layers and resources of FHIR.[34]
|
FHIR resources
A resource is the smallest discrete concept that can be independently maintained and is the lowest feasible unit of a FHIR-based transaction.[36] As a result, a resource is a known identity that provides useful data. Each resource has distinct bounds and differs from all others. A resource should be provided in sufficient depth to specify and enable the process's medical data interchange. The FHIR community has specified over 150 resources to date, according to the most recent FHIR version (R4).[37]
There are five key categories in which these resources can be found:
- Administrative: location, organization, device, patient, and group
- Clinical: CarePan, diagnostics, medication, allergy, and family history
- Financial: billing, payment, and support
- Infrastructure: conformance, document, and message profile
- Workflow: encounter, scheduling, and order
FHIR is fast gaining popularity due to its dynamic properties. FHIR is projected to quickly become a symbol for clinical data interchange in the healthcare industry.
Workflow description
Workflow is a critical component of healthcare; orders, care regimens, and referrals drive the majority of activity in inpatient settings, as well as a significant amount of activity in community care. FHIR is concerned with workflow when it is necessary to share information about workflow state or relationships, when it is necessary to coordinate or drive the execution of workflow across systems, and when it is necessary to specify permissible actions, dependencies, and behavior requirements.
Workflow state and relationships
FHIR does not have to be used for workflow execution. Orders, care plans, test findings, hospital admissions, claim payments, and other documents can all be exchanged utilizing FHIR resources without the need for a FHIR transaction to solicit fulfillment of those orders or request payment of those claims. Because it necessitates a greater level of standardization, interoperable support for workflow execution is a more advanced FHIR activity. Interoperable workflow execution necessitates the standardization of processes, roles, and activities across multiple systems, rather than just the data to be exchanged.
Even if FHIR is not used for workflow execution, there is still a requirement to standardize workflow data elements: how does an event or a result point to the order that allowed it? How are parent and child steps tied together? How does a care plan know which protocol it is following?
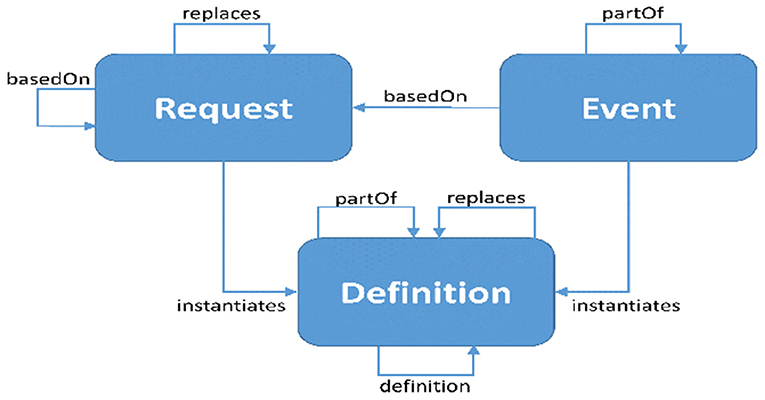
FHIR distinguishes three types of resources engaged in activities: requests, events, and definitions. Each of these categories is associated with a “pattern.” Resources in that category are encouraged to follow their specific pattern. These patterns provide conventional elements that are common to the majority of resources in each category. Work groups are anticipated to align with common domain behavior, and requirements as more authoritative than “desired” architectural patterns, and as such, strict conformance is not necessary. When a pattern capability is assessed to be “not common, but nonetheless relevant” for a given resource, it may be supplied through extensions rather than core parts. Figure 3 represents the workflow relations of the FHIR standard.[38]
|
Overview of health informatics
Health informatics involves more than merely automating routine tasks. With contemporary technology developments in machine learning and deep learning, it is possible to redesign systems using methodologies that were previously impossible or not even considered.[26] Machine learning and deep learning are computationally expensive, however, though they can now be handled by the latest IBM POWER9 processors with GPU capabilities, which was previously impossible because the data was not available in electronic form and the number of possible symptoms/incident patterns was too big to manage. Early detection of patterns that can anticipate what kind of treatment or diagnosis can be offered to such patients has improved dramatically.[39]
In the future, modern healthcare units will make use of such a framework for successful delivery of treatments for society as a whole, making effective use of data obtained from such systems by extracting insights that assist decision makers such as doctors, hospital owners, and health policymakers. However, classification and regression tree (CART) components are required for successful clinical decision support. For example, vital signs must be clearly classified to be applied to prediction.[40][41] From there, the prediction of a patient's breathing rate obtained from sensors acts as an example of regression.[42] In the future, this sort of CART-based Bayesian inference will be used to make better predictions in the domain of health informatics.
However, several not-so-commonly employed principles will have to first be implemented in informatics systems in order to answer some the most pressing future difficulties in health informatics:
- Multi-task learning: Traditional machine learning frameworks consider only one learner attempting to solve a single task. However, in many applications, there are multiple tasks that label the same data instances differently. When the tasks are related, the information learned from each task can be used to improve learning of other tasks. Learning relevant tasks concurrently, rather than learning each task independently, is thus advantageous. Multi-task learning makes use of the intrinsic relationships between multiple tasks to improve generalization performance. It benefits all tasks by leveraging task relatedness and shared information across relevant tasks.[43]
- Transfer learning: Traditional machine learning technology has had a lot of success and has been used in many practical applications, but it still has certain limits in some real-world settings. Machine learning works best when there are a lot of labeled training cases with the same distribution as the test data. In many cases, however, gathering sufficient training data is costly, time-consuming, or even impossible. Semi-supervised learning can help to alleviate this difficulty by removing the requirement for large amounts of labeled data. A semi-supervised approach typically requires a small amount of labeled data and a large amount of unlabeled data to improve learning accuracy. However, in many cases, unlabeled instances are difficult to collect, making the resulting traditional models unsatisfactory.[44]
- Multi-agent hybrid systems: Multi-agent systems are networks of interconnected autonomous agents in which the behavior of neighboring agents influences the dynamics of each agent. Because of the increasing importance of multi-agent systems, there is a growing interest in coordination control to ensure consensus, flocking, containment, formation, rendezvous, and so on. To better understand multi-agent coordination, a variety of dynamic models of agents have been developed over the last two decades. Furthermore, many mathematical methods are used in the analysis and control of multi-agent systems. For more information, see research by Qin et al.[45] and the references within the research of Zheng et al.[46]
- Representation learning: Patient-specific data such as vital signs, medications, laboratory measures, observations, clinical notes, fluid balance, procedure codes, diagnostic codes, and so on are all included in modern EHR systems. Clinicians originally employed the codes and their hierarchies, as well as their associated ontologies, for internal administrative and invoicing functions. Recent deep learning algorithms, on the other hand, have attempted to project discrete codes into vector space, identify intrinsic commonalities between medical concepts, more accurately depict patients' health, and perform more precise predicting tasks. Word embedding and unsupervised learning have been used to examine medical concepts and patient representations in general.[47]
Health informatics has a number of long-term benefits in terms of research and healthcare delivery that can be used to create a sustainable ecosystem. ICTs aid in the enrichment of relevant data for analysis and decision making by health professionals. Following the COVID-19 pandemic, new-age healthcare units will arise, with increased investment and research spending, making public healthcare more accessible. As a result, solutions are required to manage the massive amounts of data created by medical equipment and healthcare systems, allowing for effective storage and retrieval in real-time data analysis and decision making.
Informatics approaches
To make electronic health data more easily usable for research, recent publications have identified the need for effective adoption and use of standards, essential data and research services, clear and consistent policies regarding data access and use, and transparent and effective governance structures.[48][49]
To achieve data quality criteria, electronic health data utilized in research frequently require standardized ontologies, additional contextual information, field transformations, and missing or contradictory data to be handled.[50] For research-related data or functions, such as cohort identification and repeated extracts of source data over time, system development is frequently required.[49] Organizations with expertise utilizing and enhancing their health IT infrastructure for research have shared their lessons learned in these areas, adding value to organizations with similar goals but less experience or resources.[51]
For example, when preparing data for research use, organizations must understand the clinical context and structure of electronic health data, just as they do for other data uses such as decision support or population health. Individual researchers and data analysts can be relieved of their load by informatics support that spans research and operational usage of data. It is vital to evaluate and develop informatics tools and approaches by establishing processes that allow for coordinated governance and decisions informed by research users.
Investing in infrastructure to enable the use of electronic health data for research has also been shown to be beneficial to researchers by providing them with the necessary tools and expertise, to patients by providing clinical trial participation opportunities, to clinicians by enabling more rapid translation of research into practice, and to population health analysts by facilitating patient cohort views. In order to reduce project-specific IT costs, using health IT to assist research necessitates greater flexibility, increasing use of standards, and reusable ways for getting, preparing, and evaluating data.[52]
Any use of operational data in research necessitates the establishment of a privacy and security framework, as well as data governance monitoring. Two initiatives—Informatics for Integrating Biology and the Bedside (i2b2) and Observational Health Data Sciences and Informatics (OHDSI)—have developed informatics tools and approaches that allow researchers to query organizational participants and support transformation or analytics of relevant data to facilitate research.[53][54]
Specifically, i2b2 has standardized data models and distributed computational tools that enable for the anonymous identification of potential genomic study participants at the institution level. OHDSI also employs a single data model, which incorporates information such as health economics and health systems. The methodologies utilized in these programs demonstrate the kind of functionality that may be required in health IT systems to better support research, as well as the types of concerns with the quality of electronic health data that regularly arise.
Status QUO in health informatics: An Indian perspective
Health care delivery systems
Despite having a solid telecommunication infrastructure, many existing healthcare systems are based on manual record keeping. It would seem the value of health informatics in healthcare delivery has yet to be recognized by many policymakers.[55]
In countries such as India, health informatics is a new and emerging discipline. Its future prospects are very bright, thanks to the development of excellent infrastructure here. However, in order to implement a robust framework, this necessitates a multidisciplinary interaction with various stakeholders.
Information systems development could be another area where research is being conducted to improve the way data flows from various sources such as devices and medical equipment, allowing doctors and decision makers to make rational decisions on critical cases or equipment purchases in the future.
Digitizing all medical data also aids in the creation of a structure for patient-related data in a hospital that can be easily retrieved and searched. Finally, the development of some kind of EHR can be accomplished through the development of information systems.[56]
Applications of health informatics
Health informatics in India can become cost-effective and ensure proper service delivery, which aids in beneficial behavioral change through the use of ICTs.[57] We can create novel applications that can be used effectively by utilizing local talent and effective use of ICT in remote parts of India.[58] Various governance issues can be addressed in the future with certain checks and balances in the data collection and analysis process.[59] The following are some of the areas where health informatics can be used:
- Epidemiological disease prediction
- Disaster management
- Awareness in healthcare processes
- Healthcare in remote areas
- EHRs and their linkages with health systems
- Health statistics
- Education and training
- Development of clinical decision support systems (CDSS)
- Public health research
- Visualization tools for doctors
- Recommendation systems for health informatics
- Precision drug prediction
The potential of this emerging area has far-reaching benefits over a long period of time, and new and novel solutions can be built using various machine/deep learning models. There is a lot of work to be done in this area where we can use cutting-edge technology to aid/assist in the development of robust products and frameworks for public health policy.[60][61][62][63]
Future trends and directions in health informatics
There are many current trends in the field of health informatics that can be used to develop sustainable products, services, and health-related policies for effective implementation across the country and internationally. A few of them are listed below, and many more trends may emerge in the near future as a result of discussions with multiple stakeholders.
- Data standards and Interoperability
- Processes to transform medical/clinical data
- Toolkits and pipelines for data management
- Standardized reporting methodologies
- Appropriate use of informatics expertise
More trends may emerge in the future, taking into account the most recent technological advancements. Because health informatics is a new and emerging field, more research challenges may emerge, bringing forth newer perspectives. To solve more difficult problems in this area, future researchers will likely prefer machine/deep learning methods/models.[26] There are numerous other research directions being pursued in relation to various aspects of healthcare data such as quality, veracity, privacy, and timeliness. The following are some of the most notable data characteristics of healthcare data[9][64]:
1. Complexity and noise: Because healthcare data is multisource and multimodal, it has a high level of complexity and noise. Furthermore, there are issues with impurity and missing values in high-volume data. It is difficult to deal with all of these issues, both in terms of scale and accuracy, despite the fact that a number of methods have been developed to improve data accuracy and usability.[65] Because the quality of data dictates the quality of information, which in turn affects decision-making, it is vital to develop efficient big data cleansing ways to improve data quality in order to make effective and correct decisions.[66]
2. Heterogeneity: Traditional healthcare data is frequently fragmented into multiple forms due to a lack of standardization. As a result, it is both reasonable and important to investigate and adopt universal data standards. However, due to the complexity of developing universal data standards, it is a difficult undertaking. Not only is healthcare data diverse, but there are also numerous technical challenges to integrating that data for specific purposes.[67] Even with standardized data formats, the multi-modal character of data makes efficient fusion difficult[68], necessitating the development of advanced analytics that cope with vast amounts of multi-modal data. The integration and synthesis of multi-source and multi-modal healthcare data on a larger scale would be a significant issue.
3. Longitudinal analysis: Longitudinal data is the collection of repeated measurements of participant outcomes and possibly treatments or exposures[69], which means that "the outcome variable is repeatedly measured on the same individual on multiple occasions."[70] In recent decades, longitudinal data analysis, particularly statistical longitudinal data analysis, has gotten a lot of attention. Longitudinal studies are used to characterize normal growth and aging, as well as to evaluate the effectiveness of risk factors and therapies. It is extremely important in epidemiology, clinical research, and therapeutic evaluation. With big data analytic tools, it is possible to perform longitudinal care analysis across patients and diagnoses to identify the optimal care options.
4. Scale: Healthcare data is continuously expanding in quantity and scope.[68] The fact that data volume is growing faster than processing power is a significant challenge in managing vast amounts of data. Several fundamental adjustments are occurring to handle this enormous transition.[71] First, in recent years, CPU technology has increasingly turned its focus to parallel data processing within nodes and the packing of numerous sockets. Second, the shift to cloud computing allows for information sharing and the consolidation of multiple workloads into large-scale clusters. Third, the transformation of the traditional I/O subsystem from hard disk drives (HDDs) to solid-state drives (SSDs), as well as other storage technologies, is reforming data processing system design and operation.
5. Real-time requirement: The velocity of big data in health informatics reflects not only the rate of data collecting and processing, but also the timeliness of replies. There are various instances that call for a quick choice. For example, it would be immensely desirable to monitor and analyze a person's health condition in real time or near real time in order to predict potential disease. It would also be critical to raise the alert for a potential influenza outbreak by examining public health statistics. Although real-time analytic applications are still in their infancy in the big data era, they represent the strongest trend and most promising direction in health informatics' future.[72]
6. Privacy: Data privacy is another major worry for future big data analytics in health informatics.[73] Although strong laws control more formalized EHR data, extra attention should be taken and standards should be enforced to regularize the use and dissemination of personal and sensitive information obtained from diverse sources. In addition to data privacy, there are a number of other challenges— such as data protection, data security, data safety, and the protection of doctors from liability resulting from manipulated data—that necessitate the use of specialized big data analytics to address these complicated constraints.[73][74]
7. Visualization: The visualization of healthcare data is crucial for exploratory or discovery analytics, which aim to investigate and discover elements that are hidden or encrypted in the data.[75] Effective visualization tools will enable clinicians and physicians to explore data without the need for IT assistance.[72]
8. Multidisciplinary and human-computer interaction: Big data in health informatics is expected to be a multidisciplinary job requiring ongoing contributions from multiple topic experts.[76] They include, but are not limited to, engineering scientists who provide basic big data infrastructure to collect, store, share, and manage big data; computer science data scientists who provide solutions for processing and analyzing high-volume, high-velocity healthcare data using a variety of data mining and machine-learning techniques; and clinicians and physicians from the medical domain who provide professional healthcare data analysis, personalized care, and make recommendations. Computer algorithms can struggle to find patterns and interpret results at times; consequently, it is a desirable feature for an advanced big data analysis system to be able to enable input from numerous human specialists, exchange of viewpoints, and collaborative exploration of outcomes. Furthermore, in the health sector, we sometimes do not have massive data: we are confronted with a small number of datasets or unusual events, where, for example, machine-learning algorithms suffer from insufficient training samples. In such circumstances, we require more than just automatic machine learning; we also require a person in the loop. In other words, interactive machine learning (iML) or “human in the loop” techniques can be used in health informatics when automatic machine learning algorithms cannot handle rare occurrences on their own and a human expert is required to interact in the learning process.[77] The interplay between computer algorithms and human specialists has the potential to improve the learning process.
Challenges in health informatics
There are numerous challenges in this area, particularly in a country like India, where a large population is denied affordable healthcare. This can serve as a starting point for developing and implementing robust health informatics applications, products, and research and development investments. The start-up/venture costs, people, and equipment are very high, and it is a niche sector in which many people are hesitant to venture into; however, such a space/sector can be leveraged, making very good business sense.[78]
To improve the way health services are delivered and implemented to the public, a multidisciplinary approach involving various sectors/stakeholders is required. These informatics systems can be used for a variety of purposes. Medical/healthcare data will be more structured and democratized by competent authorities. The advancement of EHRs and web-based health monitoring systems will also aid in rational decision making and policy framework implementation.[12]
However, there may be numerous bottlenecks in the development of ICT systems for health informatics.[55][79] For example, the majority of stakeholders are unconvinced about the benefits of internet technologies in health care and are unfamiliar with how to use such new technology.[80] Concerns about security and privacy may also arise as robust healthcare systems are developed in the future.[12]
Proper techniques are essential to ensure patient data confidentiality, and system security may become a concern when data policy standardization increases. Many new challenges can be encountered while developing novel and innovative ways to promote public health through the use of information technology (IT) and other computing technological advances such as cloud computing, data visualization, and health informatics innovations. Future research is required because the health informatics domain is still in its early stages, where more difficult problems can be solved and newer products and services can be spawned as a business venture. Additionally, deep learning in health informatics has its own set of challenges.[26]
Additionally, despite significant investments in information technology, patient safety and productivity have not improved. Preventable medical errors are the third leading cause of death in the United States, after heart disease and cancer, killing over 400,000 people each year. These blunders cost the United States over one trillion dollars per year. To combat this problem, the federal government has mandated that the healthcare industry transition to electronic health records (EHRs) and use these records to improve patient processes and outcomes (i.e., meaningful use). Emerging economies have to allocate and give incentives to healthcare units/organizations to promote the use of EHRs.
The COVID-19 pandemic has also revealed challenges in maintaining quality patient outcomes through health information management and health informatics. Roadblocks have included a lack of standards for information exchange between providers and PHAs (public health authorities); issues with data collection and data quality, particularly in terms of completeness and timeliness; and gaps in effectiveness of governance, public policies, and regulations.
The latter in particular highlights a lack of procedures to support efficient data sharing, contact tracing, and data governance, as well as providers' concerns about privacy regulations, which resulted in insufficient data sharing. Governance and public policy hurdles stem from chronic underfunding of public health infrastructure, as well as a lack of adequate investments in resources (particularly qualified employees) and facilities. A key difficulty is also found in the lack of international coordination. Many overlapping and interrelated legal, ethical, scientific, technical, technological, health equality, and privacy elements have influenced how health information has been managed or mismanaged during the COVID-19 pandemic. Other long-standing systemic difficulties in health information management will need to be addressed in order to operationalize many of the data and information system recommendations.[81]
Another challenge in effectively implementing health informatics rests in the financial investment required to design, execute, and sustain e-health programs. For example, Anderson cited a lack of financial backing and high initial expenses as hurdles to implementing ICT in health care.[82] While health informaticians and information professionals may see future benefits from investments in ICTs, health professionals and managers may be skeptical, especially if they are satisfied with current methods of working and wish to maintain the status quo; they may see such initiatives as diverting financial resources away from under-resourced clinical care.[83]
Continued resistance to the establishment of ICT systems by health professionals and managers can lead to further issues once the systems are in place, and the restricted adoption of health informatics applications has meant that their potential is not always achieved. Decision support systems, for example, may be ignored or overridden, and evidence-based information may have limited applicability for an individual patient. Clinicians make life-changing judgments or act in life-threatening situations, and if they don't comprehend the reasons behind the decisions behind a CDSS, they won't trust it or use it effectively.[84] This highlights the importance of not only involving physicians and healthcare professionals in the construction of systems and the interpretation of outcomes, but also of providing adequate explanation and information at the point of care for healthcare practitioners to trust such systems.[84]
As previously stated, identifying the types of information that clinicians require, as well as the methods by which they access and utilize information, is critical in ensuring that developments not only meet the needs of the users, but are also perceived to be valuable, so that health professionals and other users will want to maximize their potential. Addressing healthcare professionals', patients', and the public's concerns about data security, as well as threats to patient privacy and confidentiality, will be critical in developing online access to patient records.[85] Greater security measures integrated into system design will help boost system confidence; however, the chance of third parties getting access to sensitive patient-identifiable data remains a danger.[82]
Another challenge that can stall the creation and execution of health informatics efforts is quality. The real and perceived quality of data entered into systems and then used for health care is vital not only for assuring system use, but also for the safety and well-being of patients. If data is not input, or is not entered correctly, the buildup of missing or low quality data discourages others from using the system and creates additional suspicion and skepticism about future advancements. The importance of accurate and correct data will grow as lifelong electronic records are established[84], both prospectively as individuals are born and retrospectively using data acquired over an existing person's lifetime to date.
As previously noted, the earlier development of small-scale information systems within individual departments or hospitals resulted in system incompatibility and difficulties communicating or transferring data when larger-scale systems were later built. One approach to addressing this issue is to increase interoperability and employ known electronic record architectures in the creation of new systems. In addition, the lack of data standards in health presents additional challenges for moving and sharing data between systems.[82] Attempts to address these issues include the creation of information management standards such as Digital Imaging and Communications in Medicine (DICOM), HL7, and terminologies and coding systems like the International Classification of Diseases (ICD) and SNOMED CT to standardize the ways in which medical conditions and diseases are represented in computer-based systems and codify the natural language used by medical staff. In particular, the ICD was created to provide a standard method of classifying medical diagnoses for epidemiology and healthcare purposes. Initially, it only included causes of death, but more recent versions have included causes of morbidity, and it is now in its eleventh version.[86]
Health data standards challenges and possible solutions to them
Clearly, data standards are not lacking in the healthcare industry. Standard development organizations have created a plethora of them to address nearly every facet of communication between diverse health systems. However, the simple fact that they exist and are available does not address all of the issues surrounding interoperability. What follows are some of the more difficult standards issues, as well as potential solutions.
1. Medical coding speed and accuracy issues: The manual work required to convert diagnoses, treatments, services, treatment plans, and other concepts into medical codes is undertaken by professionally qualified individuals. Computer-assisted coding systems are now used by coders. However, the translation process' speed and precision are far from flawless. To that aim, high hopes are placed on AI-powered tools capable of identifying proper codes and recommending them for expert evaluation. Currently, such intelligent systems speed up coding, but they cannot completely replace humans and automate the entire process.
2. Need for mapping between codes: Each code in healthcare serves a specific purpose. SNOMED allows physicians to provide a thorough clinical picture of a patient being treated, whereas ICD-10 presents diagnoses quickly and CPT summarizes services. However, there are times when translation from one code system to another is required. As previously stated, SNOMED cannot be used for billing reasons and must be translated to ICD-10-CT. To overcome mapping issues, standard development organizations continue to research various approaches.
3. Lack of compatibility between old and new standards: To comply with existing interoperability regulations, hospitals must make content described by USCDI available via FHIR-based APIs. However, most older EHR systems were designed with previous standards in mind. Some of them are only capable of importing and exporting HL7 v2 messages. Others rely heavily on C-CDA materials. Neither v2 nor C-CDA are compatible with granular USCDI data elements or FHIR basic interchangeable data block resources. As a result, hospitals will require additional digital technologies and human resources to extract data from legacy formats and convert it into FHIR- and USCDI-compliant formats.
4. No two-way communication between patients and EHRs: The FHIR standard enables patients to access health data through apps of their choice. However, because EHRs largely limit access to their systems as read-only, this more often than not becomes a one-way street. The software allows users to request information but does not allow them to modify or change it. Many industry experts believe that the next major difficulty for healthcare is a lack of two-way communication between medical apps and EHR systems. And, sooner or later, it will need the development of new data standards.[87]
Conclusion
Continued research in the domain of health informatics is vital, driving new discoveries that can be realized effectively and via rigorous testing. There are no proven design blueprints for such a comprehensive infrastructure, and the goal is always shifting due to the nature of real-time patient, medical, and equipment data collection from a variety of sources. The future of health informatics lies in the creation of novel algorithms, models, and an ecosystem that is conducive to health professionals and decision makers.
Some of the advantages that will result from innovation in this emerging area will be critical, including the:
- development of case- and incident-related health information standards and services;
- improvement in professionalism among healthcare units;
- creation of various innovative industrial processes;
- enhancement of research collaboration both nationally and internationally;
- development of better data visualization tools;
- development of novel prediction models using machine learning, deep learning, and reinforcement learning;
- creation of new products and services related to healthcare and health informatics;
- improvement of storage and retrieval mechanisms associated with health data; and
- development of curated, novel datasets for research communities.
Current cutting-edge health informatics research projects aim to discover new condition onset behaviors that are visible in physiological data streams earlier than traditional condition detection in critical care data.[88] Cloud computing has attracted a lot of research attention, but only a small portion of the work done so far has addressed performance issues, and only a few examinations have used a rigorous analytical approach.[89][90][91][92]
Big data is also playing an important role in health informatics, where a large amount of data related to healthcare is generated, assisting doctors and decision makers in making rational decisions regarding patient treatment and diagnosis. Newer computational technologies may emerge that will improve the way healthcare is delivered and implemented in the future, thereby vastly improving the public healthcare system. Policymakers can propose tried-and-true use cases that can be transformed into a meaningful framework in which all stakeholders can deliberate and decide on the best model for improving the public health care system.
Health informatics is a new field, with many stakeholders involved in the design and implementation of sustainable public health systems and policies for the benefit of society as a whole.
Acknowledgements
Author contributions
MY has written the manuscript with relevant information from the literature regarding the major challenges and gaps that the present health informatics system and public health system are undergoing. The manuscript was reviewed and inputs were given by JK to focus on health informatics and policy framework. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
- ↑ Jordan, M. I.; Mitchell, T. M. (17 July 2015). "Machine learning: Trends, perspectives, and prospects" (in en). Science 349 (6245): 255–260. doi:10.1126/science.aaa8415. ISSN 0036-8075. https://www.science.org/doi/10.1126/science.aaa8415.
- ↑ LeCun, Yann; Bengio, Yoshua; Hinton, Geoffrey (28 May 2015). "Deep learning" (in en). Nature 521 (7553): 436–444. doi:10.1038/nature14539. ISSN 0028-0836. http://www.nature.com/articles/nature14539.
- ↑ Stark, Pete (1 December 2010). "Congressional intent for the HITECH Act". The American Journal of Managed Care 16 (12 Suppl HIT): SP24–28. ISSN 1936-2692. PMID 21314216. https://pubmed.ncbi.nlm.nih.gov/21314216.
- ↑ Jamoom, Eric; Beatty, Paul; Bercovitz, Anita; Woodwell, David; Palso, Kathleen; Rechtsteiner, Elizabeth (1 July 2012). "Physician adoption of electronic health record systems: United States, 2011". NCHS data brief (98): 1–8. ISSN 1941-4927. PMID 23050588. https://pubmed.ncbi.nlm.nih.gov/23050588.
- ↑ Jacobs, Adam (1 August 2009). "The pathologies of big data" (in en). Communications of the ACM 52 (8): 36–44. doi:10.1145/1536616.1536632. ISSN 0001-0782. https://dl.acm.org/doi/10.1145/1536616.1536632.
- ↑ Wolfe, Patrick J. (5 November 2013). "Making sense of big data" (in en). Proceedings of the National Academy of Sciences 110 (45): 18031–18032. doi:10.1073/pnas.1317797110. ISSN 0027-8424. PMC PMC3831484. PMID 24145435. https://pnas.org/doi/full/10.1073/pnas.1317797110.
- ↑ 7.0 7.1 Herland, Matthew; Khoshgoftaar, Taghi M; Wald, Randall (1 December 2014). "A review of data mining using big data in health informatics" (in en). Journal Of Big Data 1 (1): 2. doi:10.1186/2196-1115-1-2. ISSN 2196-1115. https://journalofbigdata.springeropen.com/articles/10.1186/2196-1115-1-2.
- ↑ "Future of Health Technology Institute". Future of Health Technology Institute. http://www.fhti.org/.
- ↑ 9.0 9.1 Fang, Ruogu; Pouyanfar, Samira; Yang, Yimin; Chen, Shu-Ching; Iyengar, S. S. (28 July 2016). "Computational Health Informatics in the Big Data Age: A Survey" (in en). ACM Computing Surveys 49 (1): 1–36. doi:10.1145/2932707. ISSN 0360-0300. https://dl.acm.org/doi/10.1145/2932707.
- ↑ Institute of Medicine (U.S.), ed. (1988). The future of public health. Washington, D.C: National Academy Press. ISBN 978-0-309-03830-0.
- ↑ Chen, Jiajia; Qian, Fuliang; Yan, Wenying; Shen, Bairong (2013). "Translational Biomedical Informatics in the Cloud: Present and Future" (in en). BioMed Research International 2013: 1–8. doi:10.1155/2013/658925. ISSN 2314-6133. PMC PMC3613081. PMID 23586054. http://www.hindawi.com/journals/bmri/2013/658925/.
- ↑ 12.0 12.1 12.2 Yasnoff, William A.; OʼCarroll, Patrick W.; Koo, Denise; Linkins, Robert W.; Kilbourne, Edwin M. (2000). "Public Health Informatics: Improving and Transforming Public Health in the Information Age:" (in en). Journal of Public Health Management and Practice 6 (6): 67–75. doi:10.1097/00124784-200006060-00010. ISSN 1078-4659. http://journals.lww.com/00124784-200006060-00010.
- ↑ Gable, Carol Brignoli (1 March 1990). "A COMPENDIUM OF PUBLIC HEALTH DATA SOURCES" (in en). American Journal of Epidemiology 131 (3): 381–394. doi:10.1093/oxfordjournals.aje.a115513. ISSN 1476-6256. https://academic.oup.com/aje/article/63855/A.
- ↑ Institute of Medicine (U.S.), ed. (2003). The future of the public's health in the 21st century. Washington, D.C: National Academies Press. ISBN 978-0-309-08704-9.
- ↑ Patel, Shyamal; Park, Hyung; Bonato, Paolo; Chan, Leighton; Rodgers, Mary (1 December 2012). "A review of wearable sensors and systems with application in rehabilitation" (in en). Journal of NeuroEngineering and Rehabilitation 9 (1): 21. doi:10.1186/1743-0003-9-21. ISSN 1743-0003. PMC PMC3354997. PMID 22520559. https://jneuroengrehab.biomedcentral.com/articles/10.1186/1743-0003-9-21.
- ↑ Pedrycz, Witold; Chen, Shyi-Ming, eds. (2015). Information Granularity, Big Data, and Computational Intelligence. Studies in Big Data. 8. Cham: Springer International Publishing. doi:10.1007/978-3-319-08254-7. ISBN 978-3-319-08253-0. http://link.springer.com/10.1007/978-3-319-08254-7.
- ↑ Wu,P.Y.; Cheng, C.W.; Kaddi, C.D. et al. (1 February 2017). "–Omic and Electronic Health Record Big Data Analytics for Precision Medicine". IEEE Transactions on Biomedical Engineering 64 (2): 263–273. doi:10.1109/TBME.2016.2573285. ISSN 0018-9294. PMC PMC5859562. PMID 27740470. https://ieeexplore.ieee.org/document/7587347/.
- ↑ Yang, Hung-chih; Dasdan, Ali; Hsiao, Ruey-Lung; Parker, D. Stott (2007). "Map-reduce-merge: simplified relational data processing on large clusters" (in en). Proceedings of the 2007 ACM SIGMOD international conference on Management of data - SIGMOD '07 (Beijing, China: ACM Press): 1029–40. doi:10.1145/1247480.1247602. ISBN 978-1-59593-686-8. http://portal.acm.org/citation.cfm?doid=1247480.1247602.
- ↑ Kala Karun, A.; Chitharanjan, K. (1 April 2013). "A review on hadoop — HDFS infrastructure extensions". 2013 IEEE CONFERENCE ON INFORMATION AND COMMUNICATION TECHNOLOGIES (Thuckalay, Tamil Nadu, India: IEEE): 132–137. doi:10.1109/CICT.2013.6558077. ISBN 978-1-4673-5758-6. http://ieeexplore.ieee.org/document/6558077/.
- ↑ Mohri, Mehryar; Rostamizadeh, Afshin; Talwalkar, Ameet (2012). Foundations of machine learning. Adaptive computation and machine learning series. Cambridge, MA: MIT Press. ISBN 978-0-262-01825-8.
- ↑ Bellazzi, R; Zupan, B (1 February 2008). "Predictive data mining in clinical medicine: Current issues and guidelines" (in en). International Journal of Medical Informatics 77 (2): 81–97. doi:10.1016/j.ijmedinf.2006.11.006. https://linkinghub.elsevier.com/retrieve/pii/S1386505606002747.
- ↑ Cohen, A. M. (1 January 2005). "A survey of current work in biomedical text mining". Briefings in Bioinformatics 6 (1): 57–71. doi:10.1093/bib/6.1.57. ISSN 1467-5463. https://doi.org/10.1093/bib/6.1.57.
- ↑ Bedard, Noah; Pierce, Mark; El-Naggar, Adel; Anandasabapathy, S.; Gillenwater, Ann; Richards-Kortum, R. (1 April 2010). "Emerging Roles for Multimodal Optical Imaging in Early Cancer Detection: A Global Challenge" (in en). Technology in Cancer Research & Treatment 9 (2): 211–217. doi:10.1177/153303461000900210. ISSN 1533-0346. PMC PMC2906814. PMID 20218743. http://journals.sagepub.com/doi/10.1177/153303461000900210.
- ↑ Weissleder, Ralph; Pittet, Mikael J. (3 April 2008). "Imaging in the era of molecular oncology" (in en). Nature 452 (7187): 580–589. doi:10.1038/nature06917. ISSN 0028-0836. PMC PMC2708079. PMID 18385732. https://www.nature.com/articles/nature06917.
- ↑ Pierce, Mark C.; Javier, David J.; Richards-Kortum, Rebecca (1 November 2008). "Optical contrast agents and imaging systems for detection and diagnosis of cancer" (in en). International Journal of Cancer 123 (9): 1979–1990. doi:10.1002/ijc.23858. PMC PMC2902964. PMID 18712733. https://onlinelibrary.wiley.com/doi/10.1002/ijc.23858.
- ↑ 26.0 26.1 26.2 26.3 26.4 Ravi, Daniele; Wong, Charence; Deligianni, Fani; Berthelot, Melissa; Andreu-Perez, Javier; Lo, Benny; Yang, Guang-Zhong (1 January 2017). "Deep Learning for Health Informatics". IEEE Journal of Biomedical and Health Informatics 21 (1): 4–21. doi:10.1109/JBHI.2016.2636665. ISSN 2168-2194. http://ieeexplore.ieee.org/document/7801947/.
- ↑ Suzuki, Kenji; Yan, Pingkun; Wang, Fei; Shen, Dinggang (2012). "Machine Learning in Medical Imaging" (in en). International Journal of Biomedical Imaging 2012: 1–2. doi:10.1155/2012/123727. ISSN 1687-4188. PMC PMC3303553. PMID 22481902. http://www.hindawi.com/journals/ijbi/2012/123727/.
- ↑ Holzinger, Andreas; Biemann, Chris; Pattichis, Constantinos S.; Kell, Douglas B. (2017). What do we need to build explainable AI systems for the medical domain?. doi:10.48550/ARXIV.1712.09923. https://arxiv.org/abs/1712.09923.
- ↑ 29.0 29.1 Ribeiro, Marco Tulio; Singh, Sameer; Guestrin, Carlos (13 August 2016). ""Why Should I Trust You?": Explaining the Predictions of Any Classifier" (in en). Proceedings of the 22nd ACM SIGKDD International Conference on Knowledge Discovery and Data Mining (San Francisco California USA: ACM): 1135–1144. doi:10.1145/2939672.2939778. ISBN 978-1-4503-4232-2. https://dl.acm.org/doi/10.1145/2939672.2939778.
- ↑ Bahdanau, Dzmitry; Cho, Kyunghyun; Bengio, Yoshua (2014). Neural Machine Translation by Jointly Learning to Align and Translate. doi:10.48550/ARXIV.1409.0473. https://arxiv.org/abs/1409.0473.
- ↑ Buntin, Melinda Beeuwkes; Burke, Matthew F.; Hoaglin, Michael C.; Blumenthal, David (1 March 2011). "The Benefits Of Health Information Technology: A Review Of The Recent Literature Shows Predominantly Positive Results" (in en). Health Affairs 30 (3): 464–471. doi:10.1377/hlthaff.2011.0178. ISSN 0278-2715. http://www.healthaffairs.org/doi/10.1377/hlthaff.2011.0178.
- ↑ Menachemi, Nir; Brooks, Robert G. (1 June 2006). "Reviewing the Benefits and Costs of Electronic Health Records and Associated Patient Safety Technologies" (in en). Journal of Medical Systems 30 (3): 159–168. doi:10.1007/s10916-005-7988-x. ISSN 0148-5598. http://link.springer.com/10.1007/s10916-005-7988-x.
- ↑ King, Jennifer; Patel, Vaishali; Jamoom, Eric W.; Furukawa, Michael F. (1 February 2014). "Clinical Benefits of Electronic Health Record Use: National Findings" (in en). Health Services Research 49 (1pt2): 392–404. doi:10.1111/1475-6773.12135. PMC PMC3925409. PMID 24359580. https://onlinelibrary.wiley.com/doi/10.1111/1475-6773.12135.
- ↑ 34.0 34.1 34.2 34.3 34.4 "2.16 FHIR Overview - Architects". Health Level 7. 1 November 2019. https://www.hl7.org/fhir/overview-arch.html.
- ↑ Mandel, Joshua C; Kreda, David A; Mandl, Kenneth D; Kohane, Isaac S; Ramoni, Rachel B (1 September 2016). "SMART on FHIR: a standards-based, interoperable apps platform for electronic health records" (in en). Journal of the American Medical Informatics Association 23 (5): 899–908. doi:10.1093/jamia/ocv189. ISSN 1527-974X. PMC PMC4997036. PMID 26911829. https://academic.oup.com/jamia/article/23/5/899/2379865.
- ↑ Yan, Hangcheng; Xiao, Liang; Tian, Jingbai (2017). "Clinical Decision Support Based on FHIR Data Exchange Standard" (in en). Proceedings of the 2nd International Conference on Mechatronics Engineering and Information Technology (ICMEIT 2017) (Dalian, China: Atlantis Press). doi:10.2991/icmeit-17.2017.96. ISBN 978-94-6252-338-8. http://www.atlantis-press.com/php/paper-details.php?id=25876700.
- ↑ Sharma, Meenakshi; Aggarwal, Himanshu (2019), Krishna, C. Rama; Dutta, Maitreyee; Kumar, Rakesh, eds., "HL-7 Based Middleware Standard for Healthcare Information System: FHIR", Proceedings of 2nd International Conference on Communication, Computing and Networking (Singapore: Springer Singapore) 46: 889–899, doi:10.1007/978-981-13-1217-5_87, ISBN 978-981-13-1216-8, http://link.springer.com/10.1007/978-981-13-1217-5_87. Retrieved 2022-05-16
- ↑ 38.0 38.1 "12.5 Workflow Description". Health Level 7. 1 November 2019. https://www.hl7.org/fhir/workflow.html.
- ↑ Institute of Medicine (12 February 1999). Chemical and Biological Terrorism: Research and Development to Improve Civilian Medical Response. Washington, D.C.: National Academies Press. doi:10.17226/6364. ISBN 978-0-309-06195-7. http://www.nap.edu/catalog/6364.
- ↑ Clifton, David Andrew; Hugueny, Samuel; Tarassenko, Lionel (1 December 2011). "Novelty Detection with Multivariate Extreme Value Statistics" (in en). Journal of Signal Processing Systems 65 (3): 371–389. doi:10.1007/s11265-010-0513-6. ISSN 1939-8018. http://link.springer.com/10.1007/s11265-010-0513-6.
- ↑ Hugueny, Samuel; Clifton, David A.; Tarassenko, Lionel (2011), Fred, Ana; Filipe, Joaquim; Gamboa, Hugo, eds., "Probabilistic Patient Monitoring with Multivariate, Multimodal Extreme Value Theory", Biomedical Engineering Systems and Technologies (Berlin, Heidelberg: Springer Berlin Heidelberg) 127: 199–211, doi:10.1007/978-3-642-18472-7_16, ISBN 978-3-642-18471-0, http://link.springer.com/10.1007/978-3-642-18472-7_16. Retrieved 2022-05-16
- ↑ Meredith, D. J.; Clifton, D.; Charlton, P.; Brooks, J.; Pugh, C. W.; Tarassenko, L. (1 March 2012). "Photoplethysmographic derivation of respiratory rate: a review of relevant physiology" (in en). Journal of Medical Engineering & Technology 36 (1): 1–7. doi:10.3109/03091902.2011.638965. ISSN 0309-1902. http://www.tandfonline.com/doi/full/10.3109/03091902.2011.638965.
- ↑ Hunt, Xin J.; Emrani, Saba; Kabul, Ilknur Kaynar; Silva, Jorge (2018). Multi-Task Learning with Incomplete Data for Healthcare. doi:10.48550/ARXIV.1807.02442. https://arxiv.org/abs/1807.02442.
- ↑ Zhuang, Fuzhen; Qi, Zhiyuan; Duan, Keyu; Xi, Dongbo; Zhu, Yongchun; Zhu, Hengshu; Xiong, Hui; He, Qing (1 January 2021). "A Comprehensive Survey on Transfer Learning". Proceedings of the IEEE 109 (1): 43–76. doi:10.1109/JPROC.2020.3004555. ISSN 0018-9219. https://ieeexplore.ieee.org/document/9134370/.
- ↑ Qin, Jiahu; Ma, Qichao; Shi, Yang; Wang, Long (1 June 2017). "Recent Advances in Consensus of Multi-Agent Systems: A Brief Survey". IEEE Transactions on Industrial Electronics 64 (6): 4972–4983. doi:10.1109/TIE.2016.2636810. ISSN 0278-0046. http://ieeexplore.ieee.org/document/7776972/.
- ↑ Zheng, Yuanshi; Zhao, Qi; Ma, Jingying; Wang, Long (1 March 2019). "Second-order consensus of hybrid multi-agent systems" (in en). Systems & Control Letters 125: 51–58. doi:10.1016/j.sysconle.2019.01.009. https://linkinghub.elsevier.com/retrieve/pii/S0167691119300179.
- ↑ Kwak, Gloria Hyunjung; Hui, Pan (2019). DeepHealth: Review and challenges of artificial intelligence in health informatics. doi:10.48550/ARXIV.1909.00384. https://arxiv.org/abs/1909.00384.
- ↑ Hersh, William; Cimino, James; Payne, Philip R.O.; Embi, Peter; Logan, Judith; Weiner, Mark; Bernstam, Elmer V.; Lehmann, Harold et al. (1 October 2013). "Recommendations for the Use of Operational Electronic Health Record Data in Comparative Effectiveness Research". eGEMs (Generating Evidence & Methods to improve patient outcomes) 1 (1): 14. doi:10.13063/2327-9214.1018. ISSN 2327-9214. PMC PMC4371471. PMID 25848563. https://egems.journal.ubiquity.website//article/10.13063/2327-9214.1018/.
- ↑ 49.0 49.1 Amoozegar, J.B.; Blumenfeld, B.H.; Brown, S.L. et al. (2017). "Building data capacity for patient-centered outcomes research in HHS: A formative evaluation of 2012-2016 projects". Division of Healthcare Quality and Outcomes Office of Health Policy/ASPE/HHS. https://www.rti.org/publication/building-data-capacity-patient-centered-outcomes-research-hhs.
- ↑ Ogunyemi, Omolola I.; Meeker, Daniella; Kim, Hyeon-Eui; Ashish, Naveen; Farzaneh, Seena; Boxwala, Aziz (1 August 2013). "Identifying Appropriate Reference Data Models for Comparative Effectiveness Research (CER) Studies Based on Data from Clinical Information Systems" (in en). Medical Care 51 (Supplement 8Suppl 3): S45–S52. doi:10.1097/MLR.0b013e31829b1e0b. ISSN 0025-7079. https://journals.lww.com/00005650-201308001-00009.
- ↑ Danciu, Ioana; Cowan, James D.; Basford, Melissa; Wang, Xiaoming; Saip, Alexander; Osgood, Susan; Shirey-Rice, Jana; Kirby, Jacqueline et al. (1 December 2014). "Secondary use of clinical data: The Vanderbilt approach" (in en). Journal of Biomedical Informatics 52: 28–35. doi:10.1016/j.jbi.2014.02.003. PMC PMC4133331. PMID 24534443. https://linkinghub.elsevier.com/retrieve/pii/S1532046414000392.
- ↑ Masys, Daniel R.; Harris, Paul A.; Fearn, Paul A.; Kohane, Isaac S. (29 August 2012). "Designing a Public Square for Research Computing" (in en). Science Translational Medicine 4 (149). doi:10.1126/scitranslmed.3004032. ISSN 1946-6234. PMC PMC3725749. PMID 22932220. https://www.science.org/doi/10.1126/scitranslmed.3004032.
- ↑ Murphy, Shawn; Churchill, Susanne; Bry, Lynn; Chueh, Henry; Weiss, Scott; Lazarus, Ross; Zeng, Qing; Dubey, Anil et al. (1 September 2009). "Instrumenting the health care enterprise for discovery research in the genomic era" (in en). Genome Research 19 (9): 1675–1681. doi:10.1101/gr.094615.109. ISSN 1088-9051. PMC PMC2752136. PMID 19602638. http://genome.cshlp.org/lookup/doi/10.1101/gr.094615.109.
- ↑ Hripcsak, George; Duke, Jon D.; Shah, Nigam H.; Reich, Christian G.; Huser, Vojtech; Schuemie, Martijn J.; Suchard, Marc A.; Park, Rae Woong et al. (2015). "Observational Health Data Sciences and Informatics (OHDSI): Opportunities for Observational Researchers". Studies in Health Technology and Informatics 216: 574–578. ISSN 1879-8365. PMC 4815923. PMID 26262116. https://pubmed.ncbi.nlm.nih.gov/26262116.
- ↑ 55.0 55.1 Bodavala, R. (1998). "Evaluation of Health Management Information System in India: Need for Computerized Databases in HMIS" (PDF). Harvard School of Public Health. https://cdn1.sph.harvard.edu/wp-content/uploads/sites/114/2012/10/rp176.pdf.
- ↑ Sarbadhikari, Suptendra Nath (1 April 2005). "The State of Medical Informatics in India: A Roadmap for Optimal Organization" (in en). Journal of Medical Systems 29 (2): 125–141. doi:10.1007/s10916-005-3001-y. ISSN 0148-5598. http://link.springer.com/10.1007/s10916-005-3001-y.
- ↑ Singh, A.K.; Kohli, M.; Trell, E.; Wigertz, O.; Kohli, S. (1 April 1997). "Bhorugram (India): revisited A 4 year follow-up of a computer-based information system for distributed MCH services" (in en). International Journal of Medical Informatics 44 (2): 117–125. doi:10.1016/S1386-5056(96)01251-8. https://linkinghub.elsevier.com/retrieve/pii/S1386505696012518.
- ↑ Chandrasekhar, C. P.; Ghosh, J. (2001). "Information and communication technologies and health in low income countries: the potential and the constraints". Bulletin of the World Health Organization 79 (9): 850–855. ISSN 0042-9686. PMC 2566653. PMID 11584733. https://pubmed.ncbi.nlm.nih.gov/11584733.
- ↑ Zodpey, S. P.; Negandhi, H. N. (1 April 2008). "Contemporary issues in public health governance--an Indian perspective". Indian Journal of Public Health 52 (2): 96–99. ISSN 0019-557X. PMID 19125539. https://pubmed.ncbi.nlm.nih.gov/19125539.
- ↑ Spencer, Matt; Eickholt, Jesse; Cheng, Jianlin (1 January 2015). "A Deep Learning Network Approach to ab initio Protein Secondary Structure Prediction". IEEE/ACM Transactions on Computational Biology and Bioinformatics 12 (1): 103–112. doi:10.1109/TCBB.2014.2343960. ISSN 1545-5963. PMC PMC4348072. PMID 25750595. http://ieeexplore.ieee.org/document/6872810/.
- ↑ Quang, Daniel; Chen, Yifei; Xie, Xiaohui (1 March 2015). "DANN: a deep learning approach for annotating the pathogenicity of genetic variants" (in en). Bioinformatics 31 (5): 761–763. doi:10.1093/bioinformatics/btu703. ISSN 1367-4803. PMC PMC4341060. PMID 25338716. https://academic.oup.com/bioinformatics/article-lookup/doi/10.1093/bioinformatics/btu703.
- ↑ Zeng, Tao; Li, Rongjian; Mukkamala, Ravi; Ye, Jieping; Ji, Shuiwang (1 December 2015). "Deep convolutional neural networks for annotating gene expression patterns in the mouse brain" (in en). BMC Bioinformatics 16 (1): 147. doi:10.1186/s12859-015-0553-9. ISSN 1471-2105. PMC PMC4432953. PMID 25948335. https://bmcbioinformatics.biomedcentral.com/articles/10.1186/s12859-015-0553-9.
- ↑ Ditzler, Gregory; Polikar, Robi; Rosen, Gail (1 September 2015). "Multi-Layer and Recursive Neural Networks for Metagenomic Classification". IEEE Transactions on NanoBioscience 14 (6): 608–616. doi:10.1109/TNB.2015.2461219. ISSN 1536-1241. http://ieeexplore.ieee.org/document/7219432/.
- ↑ Raghupathi, Wullianallur; Raghupathi, Viju (1 December 2014). "Big data analytics in healthcare: promise and potential" (in en). Health Information Science and Systems 2 (1): 3. doi:10.1186/2047-2501-2-3. ISSN 2047-2501. PMC PMC4341817. PMID 25825667. http://link.springer.com/10.1186/2047-2501-2-3.
- ↑ Müller, H.; Freytag, J.-C. (2003). "Problems, Methods, and Challenges in Comprehensive Data Cleansing" (PDF). Humboldt-Universität zu Berlin zu Berlin. https://tarjomefa.com/wp-content/uploads/2015/06/3229-English.pdf.
- ↑ Holzinger, Andreas; Simonic, Klaus-Martin, eds. (2011) (in en). Information Quality in e-Health: 7th Conference of the Workgroup Human-Computer Interaction and Usability Engineering of the Austrian Computer Society, USAB 2011, Graz, Austria, November 25-26, 2011. Proceedings. Lecture Notes in Computer Science. 7058. Berlin, Heidelberg: Springer Berlin Heidelberg. doi:10.1007/978-3-642-25364-5. ISBN 978-3-642-25363-8. http://link.springer.com/10.1007/978-3-642-25364-5.
- ↑ Richesson, Rachel L.; Krischer, Jeffrey (1 November 2007). "Data Standards in Clinical Research: Gaps, Overlaps, Challenges and Future Directions" (in en). Journal of the American Medical Informatics Association 14 (6): 687–696. doi:10.1197/jamia.M2470. ISSN 1527-974X. PMC PMC2213488. PMID 17712081. https://academic.oup.com/jamia/article/14/6/687/750453.
- ↑ 68.0 68.1 Kambatla, Karthik; Kollias, Giorgos; Kumar, Vipin; Grama, Ananth (1 July 2014). "Trends in big data analytics" (in en). Journal of Parallel and Distributed Computing 74 (7): 2561–2573. doi:10.1016/j.jpdc.2014.01.003. https://linkinghub.elsevier.com/retrieve/pii/S0743731514000057.
- ↑ Fitzmaurice, Garrett M.; Ravichandran, Caitlin (4 November 2008). "A Primer in Longitudinal Data Analysis". Circulation 118 (19): 2005–2010. doi:10.1161/CIRCULATIONAHA.107.714618. https://www.ahajournals.org/doi/10.1161/CIRCULATIONAHA.107.714618.
- ↑ Verhagen, Evert; van der Beek, Allard; Twisk, Jos; Bouter, Lex; Bahr, Roald; van Mechelen, Willem (1 September 2004). "The Effect of a Proprioceptive Balance Board Training Program for the Prevention of Ankle Sprains: A Prospective Controlled Trial" (in en). The American Journal of Sports Medicine 32 (6): 1385–1393. doi:10.1177/0363546503262177. ISSN 0363-5465. http://journals.sagepub.com/doi/10.1177/0363546503262177.
- ↑ Labrinidis, Alexandros; Jagadish, H. V. (1 August 2012). "Challenges and opportunities with big data" (in en). Proceedings of the VLDB Endowment 5 (12): 2032–2033. doi:10.14778/2367502.2367572. ISSN 2150-8097. https://dl.acm.org/doi/10.14778/2367502.2367572.
- ↑ 72.0 72.1 Elgendy, Nada; Elragal, Ahmed (2014), Perner, Petra, ed., "Big Data Analytics: A Literature Review Paper", Advances in Data Mining. Applications and Theoretical Aspects (Cham: Springer International Publishing) 8557: 214–227, doi:10.1007/978-3-319-08976-8_16, ISBN 978-3-319-08975-1, http://link.springer.com/10.1007/978-3-319-08976-8_16. Retrieved 2022-05-16
- ↑ 73.0 73.1 Weippl, Edgar R. (2005). Security in e-learning. Advances in information security. New York, NY: Springer. ISBN 978-0-387-24341-2.
- ↑ Kieseberg, Peter; Schantl, Johannes; Frühwirt, Peter; Weippl, Edgar; Holzinger, Andreas (2015), Guo, Yike; Friston, Karl; Aldo, Faisal et al.., eds., "Witnesses for the Doctor in the Loop" (in en), Brain Informatics and Health (Cham: Springer International Publishing) 9250: 369–378, doi:10.1007/978-3-319-23344-4_36, ISBN 978-3-319-23343-7, http://link.springer.com/10.1007/978-3-319-23344-4_36. Retrieved 2022-05-16
- ↑ Jeanquartier, Fleur; Holzinger, Andreas (2013), Cuzzocrea, Alfredo; Kittl, Christian; Simos, Dimitris E. et al.., eds., "On Visual Analytics and Evaluation in Cell Physiology: A Case Study", Availability, Reliability, and Security in Information Systems and HCI (Berlin, Heidelberg: Springer Berlin Heidelberg) 8127: 495–502, doi:10.1007/978-3-642-40511-2_36, ISBN 978-3-642-40510-5, http://link.springer.com/10.1007/978-3-642-40511-2_36. Retrieved 2022-05-16
- ↑ Chen, Min; Mao, Shiwen; Liu, Yunhao (1 April 2014). "Big Data: A Survey" (in en). Mobile Networks and Applications 19 (2): 171–209. doi:10.1007/s11036-013-0489-0. ISSN 1383-469X. http://link.springer.com/10.1007/s11036-013-0489-0.
- ↑ Holzinger, Andreas (1 June 2016). "Interactive machine learning for health informatics: when do we need the human-in-the-loop?" (in en). Brain Informatics 3 (2): 119–131. doi:10.1007/s40708-016-0042-6. ISSN 2198-4018. PMC PMC4883171. PMID 27747607. http://link.springer.com/10.1007/s40708-016-0042-6.
- ↑ Solberg, Kristin Elisabeth (1 January 2008). "Telemedicine set to grow in India over the next 5 years" (in en). The Lancet 371 (9606): 17–18. doi:10.1016/S0140-6736(08)60052-5. https://linkinghub.elsevier.com/retrieve/pii/S0140673608600525.
- ↑ eHealth Network (June 2008). "Universalising healthcare through telemedicine". eHealth. Elets Technomedia Pvt. Ltd. https://ehealth.eletsonline.com/2008/06/universalising-healthcare-through-telemedicine/.
- ↑ Saxena, G.; Singh, J.P. (2003). "E-medicine in India: Hurdles and future prospects". https://www.themanager.org/Resources/Telemed.pdf.
- ↑ Massoudi, Barbara L.; Sobolevskaia, Diana (1 August 2021). "Keep Moving Forward: Health Informatics and Information Management beyond the COVID-19 Pandemic" (in en). Yearbook of Medical Informatics 30 (01): 075–083. doi:10.1055/s-0041-1726499. ISSN 0943-4747. PMC PMC8416200. PMID 34479380. http://www.thieme-connect.de/DOI/DOI?10.1055/s-0041-1726499.
- ↑ 82.0 82.1 82.2 Anderson, James G. (1 May 2007). "Social, ethical and legal barriers to e-health". International Journal of Medical Informatics 76 (5-6): 480–483. doi:10.1016/j.ijmedinf.2006.09.016. ISSN 1386-5056. PMID 17064955. https://pubmed.ncbi.nlm.nih.gov/17064955.
- ↑ Wyatt, J. C (9 June 2001). "The new NHS information technology strategy". BMJ 322 (7299): 1378–1379. doi:10.1136/bmj.322.7299.1378. PMC PMC1120460. PMID 11397729. https://www.bmj.com/lookup/doi/10.1136/bmj.322.7299.1378.
- ↑ 84.0 84.1 84.2 Berner, Eta S.; Moss, Jacqueline (1 November 2005). "Informatics Challenges for the Impending Patient Information Explosion" (in en). Journal of the American Medical Informatics Association 12 (6): 614–617. doi:10.1197/jamia.M1873. ISSN 1067-5027. PMC PMC1294032. PMID 16049224. https://academic.oup.com/jamia/article-lookup/doi/10.1197/jamia.M1873.
- ↑ Becker, Moritz Y. (1 May 2007). "Information governance in NHS's NPfIT: A case for policy specification" (in en). International Journal of Medical Informatics 76 (5-6): 432–437. doi:10.1016/j.ijmedinf.2006.09.008. https://linkinghub.elsevier.com/retrieve/pii/S1386505606002139.
- ↑ "International Statistical Classification of Diseases and Related Health Problems (ICD)". World Health Organization. https://www.who.int/standards/classifications/classification-of-diseases.
- ↑ "Data Standards in Healthcare: Codes, Documents, and Exchange Formats". Altexsoft Blog. Altexsoft. 23 October 2020. https://www.altexsoft.com/blog/data-standards-healthcare/.
- ↑ McGregor, Carolyn (1 June 2013). "Big Data in Neonatal Intensive Care". Computer 46 (6): 54–59. doi:10.1109/MC.2013.157. ISSN 0018-9162. http://ieeexplore.ieee.org/document/6513228/.
- ↑ Iosup, A; Ostermann, S; Yigitbasi, M N; Prodan, R; Fahringer, T; Epema, D H J (1 June 2011). "Performance Analysis of Cloud Computing Services for Many-Tasks Scientific Computing". IEEE Transactions on Parallel and Distributed Systems 22 (6): 931–945. doi:10.1109/TPDS.2011.66. ISSN 1045-9219. http://ieeexplore.ieee.org/document/5719609/.
- ↑ Deelman, Ewa; Singh, Gurmeet; Livny, Miron; Berriman, Bruce; Good, John (1 November 2008). "The cost of doing science on the cloud: The Montage example". 2008 SC - International Conference for High Performance Computing, Networking, Storage and Analysis (Austin, TX, USA: IEEE): 1–12. doi:10.1109/SC.2008.5217932. ISBN 978-1-4244-2834-2. http://ieeexplore.ieee.org/document/5217932/.
- ↑ Wang, Lei; Zhan, Jianfeng; Shi, Weisong; Liang, Yi; Yuan, Lin (2009). "In cloud, do MTC or HTC service providers benefit from the economies of scale?" (in en). Proceedings of the 2nd Workshop on Many-Task Computing on Grids and Supercomputers - MTAGS '09 (Portland, Oregon: ACM Press): 1–10. doi:10.1145/1646468.1646475. ISBN 978-1-60558-714-1. http://portal.acm.org/citation.cfm?doid=1646468.1646475.
- ↑ Alam, S.; Barrett, R.; Bast, M.; Fahey, M.R.; Kuehn, J.; McCurdy, C.; Rogers, J.; Roth, P. et al. (1 November 2008). "Early evaluation of IBM BlueGene/P". 2008 SC - International Conference for High Performance Computing, Networking, Storage and Analysis (Austin, TX: IEEE): 1–12. doi:10.1109/SC.2008.5214725. ISBN 978-1-4244-2834-2. http://ieeexplore.ieee.org/document/5214725/.
Notes
This presentation is faithful to the original, with only a few minor changes to presentation. In some cases important information was missing from the references, and that information was added. Some grammar and sentence placement was cleaned up for better readability. A few sentences and citations were removed for their lack of relevance to the topic.