Difference between revisions of "Journal:Heart failure and healthcare informatics"
Shawndouglas (talk | contribs) (Finished adding rest of content.) |
Shawndouglas (talk | contribs) m (→Clinical practice and evidence-based management of heart failure: Internal link) |
||
| Line 24: | Line 24: | ||
==Clinical practice and evidence-based management of heart failure== | ==Clinical practice and evidence-based management of heart failure== | ||
[[Heart failure]], perhaps more than any other condition, exemplifies the potential for [[healthcare informatics]] to bridge the gap between practice and evidence-based care. The prevalence of heart failure is already estimated at one to two percent and is increasing with our ageing population.<ref name="MosterdClinical07">{{cite journal |title=Clinical epidemiology of heart failure |journal=Heart |author=Mosterd, A.; Hoes, A.W. |volume=93 |issue=9 |page=1137–46 |year=2007 |doi=10.1136/hrt.2003.025270 |pmid=17699180 |pmc=PMC1955040}}</ref> Indeed, recent work has demonstrated that incident heart failure cases exceed the four most common causes of cancer combined in the United Kingdom.<ref name="ConradTemporal18">{{cite journal |title=Temporal trends and patterns in heart failure incidence: A population-based study of four million individuals |journal=Lancet |author=Conrad, N.; Judge, A.; Tran, J. et al. |volume=391 |issue=10120 |page=572–580 |year=2018 |doi=10.1016/S0140-6736(17)32520-5 |pmid=29174292 |pmc=PMC5814791}}</ref> Moreover, decompensated heart failure accounts for up to five percent of all acute unscheduled [[hospital]] admissions and has the longest length of stay of any cardiac condition.<ref name="BHFHeart19">{{cite web |url=https://www.bhf.org.uk/what-we-do/our-research/heart-statistics |title=Heart statistics |author=British Heart Foundation |date=2019 |accessdate=13 March 2019}}</ref><ref name="BerryEcon01">{{cite journal |title=Economics of chronic heart failure |journal=European Journal of Heart Failure |author=Berry, C.; Murdoch, D.R.; McMurray, J.J. |volume=3 |issue=3 |page=283–91 |year=2001 |doi=10.1016/s1388-9842(01)00123-4 |pmid=11377998}}</ref> Given the high rates of debilitating symptoms and death associated with heart failure, this burden to both patients and healthcare systems provides a moral and financial imperative to ensure optimal delivery of proven therapies. The treatment of chronic heart failure has one of the most robust evidence bases in clinical medicine, with multiple landmark trials leading to comprehensive guidelines.<ref name="Ponikowski2016_16">{{cite journal |title=2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). Developed with the special contribution of the Heart Failure Association (HFA) of the ESC |journal=European Journal of Heart Failure |author=Ponikowski, P.; Voors, A.A.; Anker, S.D. et al. |volume=18 |issue=8 |page=891–975 |year=2016 |doi=10.1002/ejhf.592 |pmid=27207191}}</ref><ref name="NCGCAcute14">{{cite web |url=https://www.ncbi.nlm.nih.gov/books/NBK248063/ |title=Acute Heart Failure: Diagnosing and Managing Acute Heart Failure in Adults |work=NICE Clinical Guidelines, No. 187 |author=National Institute for Health and Care Excellence |publisher=National Clinical Guideline Centre |date=2014 |pmid=25340219}}</ref> Yet, despite effective therapies for heart failure being widely available, there is ample evidence to suggest a significant gap exists between guideline-directed practice and clinical practice.<ref name="ClelandManage02">{{cite journal |title=Management of heart failure in primary care (the IMPROVEMENT of Heart Failure Programme): An international survey |journal=The Lancet |author=Cleland, J.G.; Cohen-Solal, A.; Aguilar, J.C.; et al. |volume=360 |issue=9346 |pages=1631–9 |year=2002 |doi=10.1016/s0140-6736(02)11601-1 |pmid=12457785}}</ref><ref name="TengPrescrib18">{{cite journal |title=Prescribing patterns of evidence-based heart failure pharmacotherapy and outcomes in the ASIAN-HF registry: A cohort study |journal=The Lancet Global Health |author=Teng, T.K.; Tromp, J.; Tay, W.T. et al. |volume=6 |issue=9 |pages=e1008–e1018 |year=2018 |doi=10.1016/S2214-109X(18)30306-1 |pmid=30103979}}</ref><ref name="ButlerClin19">{{cite journal |title=Clinical Course of Patients With Worsening Heart Failure With Reduced Ejection Fraction |journal=Journal of the American College of Cardiology |author=Butler, J.; Yang, M.; Manzi, M.A. et al. |volume=73 |issue=8 |pages=935–44 |year=2019 |doi=10.1016/j.jacc.2018.11.049 |pmid=30819362}}</ref> | [[Heart failure]], perhaps more than any other condition, exemplifies the potential for [[Health informatics|healthcare informatics]] to bridge the gap between practice and evidence-based care. The prevalence of heart failure is already estimated at one to two percent and is increasing with our ageing population.<ref name="MosterdClinical07">{{cite journal |title=Clinical epidemiology of heart failure |journal=Heart |author=Mosterd, A.; Hoes, A.W. |volume=93 |issue=9 |page=1137–46 |year=2007 |doi=10.1136/hrt.2003.025270 |pmid=17699180 |pmc=PMC1955040}}</ref> Indeed, recent work has demonstrated that incident heart failure cases exceed the four most common causes of cancer combined in the United Kingdom.<ref name="ConradTemporal18">{{cite journal |title=Temporal trends and patterns in heart failure incidence: A population-based study of four million individuals |journal=Lancet |author=Conrad, N.; Judge, A.; Tran, J. et al. |volume=391 |issue=10120 |page=572–580 |year=2018 |doi=10.1016/S0140-6736(17)32520-5 |pmid=29174292 |pmc=PMC5814791}}</ref> Moreover, decompensated heart failure accounts for up to five percent of all acute unscheduled [[hospital]] admissions and has the longest length of stay of any cardiac condition.<ref name="BHFHeart19">{{cite web |url=https://www.bhf.org.uk/what-we-do/our-research/heart-statistics |title=Heart statistics |author=British Heart Foundation |date=2019 |accessdate=13 March 2019}}</ref><ref name="BerryEcon01">{{cite journal |title=Economics of chronic heart failure |journal=European Journal of Heart Failure |author=Berry, C.; Murdoch, D.R.; McMurray, J.J. |volume=3 |issue=3 |page=283–91 |year=2001 |doi=10.1016/s1388-9842(01)00123-4 |pmid=11377998}}</ref> Given the high rates of debilitating symptoms and death associated with heart failure, this burden to both patients and healthcare systems provides a moral and financial imperative to ensure optimal delivery of proven therapies. The treatment of chronic heart failure has one of the most robust evidence bases in clinical medicine, with multiple landmark trials leading to comprehensive guidelines.<ref name="Ponikowski2016_16">{{cite journal |title=2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). Developed with the special contribution of the Heart Failure Association (HFA) of the ESC |journal=European Journal of Heart Failure |author=Ponikowski, P.; Voors, A.A.; Anker, S.D. et al. |volume=18 |issue=8 |page=891–975 |year=2016 |doi=10.1002/ejhf.592 |pmid=27207191}}</ref><ref name="NCGCAcute14">{{cite web |url=https://www.ncbi.nlm.nih.gov/books/NBK248063/ |title=Acute Heart Failure: Diagnosing and Managing Acute Heart Failure in Adults |work=NICE Clinical Guidelines, No. 187 |author=National Institute for Health and Care Excellence |publisher=National Clinical Guideline Centre |date=2014 |pmid=25340219}}</ref> Yet, despite effective therapies for heart failure being widely available, there is ample evidence to suggest a significant gap exists between guideline-directed practice and clinical practice.<ref name="ClelandManage02">{{cite journal |title=Management of heart failure in primary care (the IMPROVEMENT of Heart Failure Programme): An international survey |journal=The Lancet |author=Cleland, J.G.; Cohen-Solal, A.; Aguilar, J.C.; et al. |volume=360 |issue=9346 |pages=1631–9 |year=2002 |doi=10.1016/s0140-6736(02)11601-1 |pmid=12457785}}</ref><ref name="TengPrescrib18">{{cite journal |title=Prescribing patterns of evidence-based heart failure pharmacotherapy and outcomes in the ASIAN-HF registry: A cohort study |journal=The Lancet Global Health |author=Teng, T.K.; Tromp, J.; Tay, W.T. et al. |volume=6 |issue=9 |pages=e1008–e1018 |year=2018 |doi=10.1016/S2214-109X(18)30306-1 |pmid=30103979}}</ref><ref name="ButlerClin19">{{cite journal |title=Clinical Course of Patients With Worsening Heart Failure With Reduced Ejection Fraction |journal=Journal of the American College of Cardiology |author=Butler, J.; Yang, M.; Manzi, M.A. et al. |volume=73 |issue=8 |pages=935–44 |year=2019 |doi=10.1016/j.jacc.2018.11.049 |pmid=30819362}}</ref> | ||
==Utilizing routinely collected healthcare data in heart failure== | ==Utilizing routinely collected healthcare data in heart failure== | ||
Latest revision as of 18:45, 23 July 2019
| Full article title | Heart failure and healthcare informatics |
|---|---|
| Journal | PLOS Medicine |
| Author(s) | Anwar, Mohamed S.; Japp, Alan G.; Mills, Nicholas L. |
| Author affiliation(s) | BHF Centre for Cardiovascular Science at University of Edinburgh |
| Primary contact | Email: nick dot mills at ed dot ac dot uk |
| Year published | 2019 |
| Volume and issue | 16 (5) |
| Page(s) | e1002806 |
| DOI | 10.1371/journal.pmed.1002806 |
| ISSN | 1549-1676 |
| Distribution license | Creative Commons Attribution 4.0 International |
| Website | https://journals.plos.org/plosmedicine/article?id=10.1371/journal.pmed.1002806 |
| Download | https://journals.plos.org/plosmedicine/article/file?id=10.1371/journal.pmed.1002806&type=printable (PDF) |
Introduction
As biomedical research expands our armory of effective, evidence-based therapies, there is a corresponding need for high-quality implementation science—the study of strategies to integrate and embed research advances into clinical practice.[1] Large-scale collection and analysis of routinely collected healthcare data may facilitate this in three main ways. Firstly, evaluation of key healthcare metrics can help to identify the areas of practice that differ most from guideline recommendations. Secondly, with sufficiently granular data, it may be possible to detect the underlying drivers of deficiencies in practice. Thirdly, longitudinal data collection should enable us to evaluate large-scale policy initiatives and compare the effectiveness of differing strategies on process and patient outcomes.
Clinical practice and evidence-based management of heart failure
Heart failure, perhaps more than any other condition, exemplifies the potential for healthcare informatics to bridge the gap between practice and evidence-based care. The prevalence of heart failure is already estimated at one to two percent and is increasing with our ageing population.[2] Indeed, recent work has demonstrated that incident heart failure cases exceed the four most common causes of cancer combined in the United Kingdom.[3] Moreover, decompensated heart failure accounts for up to five percent of all acute unscheduled hospital admissions and has the longest length of stay of any cardiac condition.[4][5] Given the high rates of debilitating symptoms and death associated with heart failure, this burden to both patients and healthcare systems provides a moral and financial imperative to ensure optimal delivery of proven therapies. The treatment of chronic heart failure has one of the most robust evidence bases in clinical medicine, with multiple landmark trials leading to comprehensive guidelines.[6][7] Yet, despite effective therapies for heart failure being widely available, there is ample evidence to suggest a significant gap exists between guideline-directed practice and clinical practice.[8][9][10]
Utilizing routinely collected healthcare data in heart failure
In PLOS Medicine, Rahimi and colleagues report the results of a longitudinal analysis of diagnostic tests, drug prescriptions, and follow-up patterns in 93,000 individuals with heart failure in the U.K.[11] The authors show convincingly that some aspects of care, such as the use of diagnostic testing and initiation of evidence-based therapies, have improved over time. Between 2002 and 2014, natriuretic peptide testing was introduced, and the use of echocardiography increased from 17% to 62%. Similarly, the initiation of combination therapy with a beta blocker and angiotensin-converting enzyme (ACE) inhibitor or angiotensin receptor antagonist increased three-fold. However, other key elements of care, such as dose titration of heart failure therapy, remained poor, and only one in five patients were followed up in primary care, with the rates declining over the study period. A notable strength of the work is the use of both primary and secondary care data within a large and relatively undifferentiated population. This approach ensures that insights from the study are applicable to a general heart failure population and reflect overall care provision.
By comparing data across a range of demographic subgroups, the authors hint at factors that may contribute to suboptimal practice. They note deficiencies in a range of quality indicators for women, older patients, and those of low socioeconomic status. It is clear how such findings, if sufficiently robust, could be used to inform future targeted interventions. The study certainly provides us valuable retrospective insights into two major policy initiatives designed to improve standards in heart failure treatment focused on primary and secondary care.[11] The data show persuasively that both the "quality and outcomes framework," a primary care reporting and incentives scheme, and the "national heart failure audit" initiative, a secondary care reporting program, changed behavior; however, the outcomes were tied too tightly to specific measures and may have led to unintended consequences. In many respects, it is not surprising that a system designed to reward initiation of heart failure treatments but not subsequent dose optimization would generate an increase in the former and a decline in the latter. Furthermore, there was a paradoxical decline in the recording of heart failure diagnosis in primary care from 56% to 36%, whereas the diagnosis in secondary care increased steadily. It is possible that practices did not register those patients who would not achieve all management recommendations, in order to maintain high adherence rates. This is a critical lesson to bear in mind whenever policies are geared to improve surrogate markers of quality rather than actual clinical outcomes.
Notwithstanding these strengths, the study does have several limitations. Although it is apparent which components of heart failure care were suboptimal, the data are insufficient in their granularity to detect the drivers for these deficiencies and to evaluate some of the key findings. Specifically, the absence of measures of symptom status, heart rate, blood pressure, left ventricular ejection fraction, comorbidity, and renal function prevent a complete interpretation of the appropriateness of prescribing. Depending on these parameters, initiation or up-titration of heart failure therapies may not have been indicated or may even have been contraindicated. Therefore, the gap between guideline-directed therapy and practice may, in many cases, reflect optimal individualized therapy and sensible clinical judgement rather than systematic deficiencies in care. This point is particularly pertinent to the disparities in prescribing in the elderly, for whom multimorbidity is common. The low rate of follow-up in both primary and secondary care is difficult to interpret in the absence of information from community heart failure programs, which comprise an essential component of heart failure care delivery. Finally, the insights into the effectiveness of policy initiatives, though interesting, are frustratingly retrospective and in some ways serve mainly to highlight the missed opportunities over the last decade. Moving forward, it is imperative to build a healthcare data infrastructure that is dynamic and can provide insights into contemporary clinical practice.
Healthcare informatics for the delivery of optimal patient-centered care
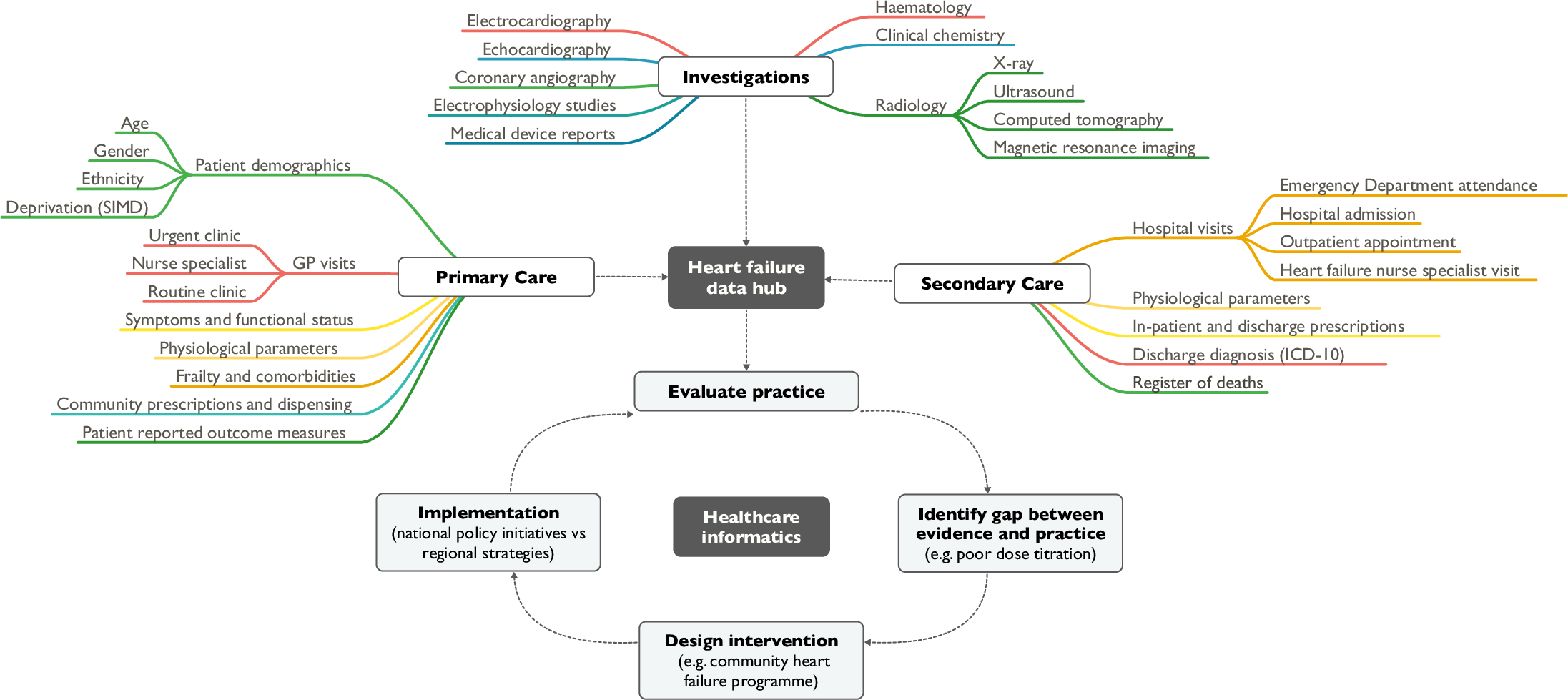
Our ability to positively impact on current disparities in care are limited because of the absence of comprehensive and contemporary data from across the spectrum of care settings. Insufficiently detailed data impede our ability to identify the causes of disparity in care and, crucially, to determine whether we are providing optimal care on an individualized basis. To successfully overcome these challenges, we need to collate healthcare data from across both primary and secondary care settings in real time and use robust methodology to evaluate major changes in clinical practice or policy decisions.[12] A platform for sharing data between primary and secondary care that is linked, anonymized, and sufficiently granular to facilitate a meaningful evaluation of current practice is required (Fig 1). This approach should be adopted widely in healthcare systems such as the National Health Service to ensure we are providing the highest standards of care for all our patients and using resources most effectively.
|
Abbreviations
- ACE, angiotensin-converting enzyme
- GP, general practitioner
- ICD-10, International Classification of Diseases-10
- SIMD, Scottish Index of Multiple Deprivation
Acknowledgements
Funding
NLM is supported by the Butler Senior Clinical Research Fellowship from the British Heart Foundation (FS/16/14/32023). AGJ is supported by a National Research Scotland Clinician Scientist Award. MSA and AGJ are supported by a Catalytic Grant from the Chief Scientist Office of the Scottish Government Health and Social Care Directorate (CGA/19/01). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Competing interests
I have read the journal's policy and the authors of this manuscript have the following competing interests: NLM has received honoraria and the University of Edinburgh has received research grants from Abbott Diagnostics and Siemens Healthineers, who manufacture diagnostic tests for heart failure. MSA and AGJ have no competing interests.
References
- ↑ Bauer, M.S.; Damschroder, L.; Hagedorn, H. et al. (2015). "An introduction to implementation science for the non-specialist". BMC Psychology 3: 32. doi:10.1186/s40359-015-0089-9. PMC PMC4573926. PMID 26376626. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4573926.
- ↑ Mosterd, A.; Hoes, A.W. (2007). "Clinical epidemiology of heart failure". Heart 93 (9): 1137–46. doi:10.1136/hrt.2003.025270. PMC PMC1955040. PMID 17699180. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1955040.
- ↑ Conrad, N.; Judge, A.; Tran, J. et al. (2018). "Temporal trends and patterns in heart failure incidence: A population-based study of four million individuals". Lancet 391 (10120): 572–580. doi:10.1016/S0140-6736(17)32520-5. PMC PMC5814791. PMID 29174292. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5814791.
- ↑ British Heart Foundation (2019). "Heart statistics". https://www.bhf.org.uk/what-we-do/our-research/heart-statistics. Retrieved 13 March 2019.
- ↑ Berry, C.; Murdoch, D.R.; McMurray, J.J. (2001). "Economics of chronic heart failure". European Journal of Heart Failure 3 (3): 283–91. doi:10.1016/s1388-9842(01)00123-4. PMID 11377998.
- ↑ Ponikowski, P.; Voors, A.A.; Anker, S.D. et al. (2016). "2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). Developed with the special contribution of the Heart Failure Association (HFA) of the ESC". European Journal of Heart Failure 18 (8): 891–975. doi:10.1002/ejhf.592. PMID 27207191.
- ↑ National Institute for Health and Care Excellence (2014). "Acute Heart Failure: Diagnosing and Managing Acute Heart Failure in Adults". NICE Clinical Guidelines, No. 187. National Clinical Guideline Centre. PMID 25340219. https://www.ncbi.nlm.nih.gov/books/NBK248063/.
- ↑ Cleland, J.G.; Cohen-Solal, A.; Aguilar, J.C.; et al. (2002). "Management of heart failure in primary care (the IMPROVEMENT of Heart Failure Programme): An international survey". The Lancet 360 (9346): 1631–9. doi:10.1016/s0140-6736(02)11601-1. PMID 12457785.
- ↑ Teng, T.K.; Tromp, J.; Tay, W.T. et al. (2018). "Prescribing patterns of evidence-based heart failure pharmacotherapy and outcomes in the ASIAN-HF registry: A cohort study". The Lancet Global Health 6 (9): e1008–e1018. doi:10.1016/S2214-109X(18)30306-1. PMID 30103979.
- ↑ Butler, J.; Yang, M.; Manzi, M.A. et al. (2019). "Clinical Course of Patients With Worsening Heart Failure With Reduced Ejection Fraction". Journal of the American College of Cardiology 73 (8): 935–44. doi:10.1016/j.jacc.2018.11.049. PMID 30819362.
- ↑ 11.0 11.1 Conrad, N.; Judge, A.; Canoy, D. et al. (2019). "Diagnostic tests, drug prescriptions, and follow-up patterns after incident heart failure: A cohort study of 93,000 UK patients". PLOS Medicine 16 (5): e1002805. doi:10.1371/journal.pmed.1002805. PMC PMC6528949. PMID 31112552. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6528949.
- ↑ Shah, A.S.V.; Anand, A.; Strachan, F.E. et al. (2018). "High-sensitivity troponin in the evaluation of patients with suspected acute coronary syndrome: A stepped-wedge, cluster-randomised controlled trial". The Lancet 392 (10151): 919–28. doi:10.1016/S0140-6736(18)31923-8. PMC PMC6137538. PMID 30170853. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6137538.
Notes
This presentation is faithful to the original, with only a few minor changes to presentation. Additional citation information such as PMID was provided when missing, and updates of content to American English were made.