Cannabinol
This article needs additional citations for verification. (October 2025) |
 | |
 | |
| Legal status | |
|---|---|
| Legal status |
|
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.216.772 |
| Chemical and physical data | |
| Formula | C21H26O2 |
| Molar mass | 310.437 g·mol−1 |
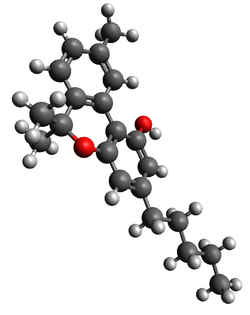
| 3D model (JSmol) | |
| Melting point | 76–77 °C (169–171 °F) [1] |
| Solubility in water | Insoluble in water,[2] soluble in methanol[3] and ethanol[4] mg/mL (20 °C) |
| |
| |
| | |
Cannabinol (CBN) is a mildly psychoactive phytocannabinoid that acts as a low affinity partial agonist at the CB1 and CB2 receptors of the endocannabinoid system (ECS).
Although CBN shares the same mechanism of action as other phytocannabinoids (e.g., Delta-9-tetrahydrocannabinol, Δ9-THC), it has a lower affinity for CB1 receptors, meaning that much higher doses of CBN are required in order to experience effects, such as mild sedation.
It was the first cannabinoid to be isolated from plants of genus Cannabis and was discovered in 1896.
Pharmacology
Pharmacodynamics
Both THC and CBN activate the CB1 (Ki = 211.2 nM) and CB2 (Ki = 126.4 nM) receptors.[5] Each compound acts as a low affinity partial agonist at CB1 receptors with THC demonstrating 5x–10× greater affinity to the CB1 receptor.[5][6][7][8][9][10] Like THC, CBN has a higher selectivity for CB2 receptors[5][8] which are located throughout the central and peripheral nervous system, but are primarily associated with immune function. CB2 receptors are known to be located on immune cells throughout the body, including macrophages, T cells, and B cells. These immune cells have been shown to decrease production of immune-related chemical signals (e.g., cytokines) or undergo apoptosis as a consequence of CB2 agonism by CBN.[11] In cell culture, CBN demonstrates antimicrobial effects, particularly in instances of antibiotic-resistant bacteria.[12] CBN has also been reported to act as an ANKTM1 channel agonist at high concentrations (>20nM).[6] While some phytocannabinoids have been shown to interact with nociceptive and immune-related signaling via transient receptor potential channels (e.g., TRPV1 and TRPM8), there is currently limited evidence to suggest that CBN acts in this way.[6][13] In preclinical rodent studies, CBN, anandamide and other CB1 agonists have demonstrated inhibitory effects on GI motility, reversible via CB1R blockade (i.e., antagonism).[6]
In considering the efficacy of cannabis-based products, there remains controversy surrounding a concept termed “the entourage effect”. This concept describes a widely reported but poorly-understood synergistic effect of certain cannabinoids when phytocannabinoids are coadministered with other naturally occurring chemical compounds in the cannabis plant (e.g., flavonoids, terpenoids, alkaloids). This entourage effect is often cited to explain the superior efficacy observed in some studies of whole-plant-derived cannabis therapeutics as compared to isolated or synthesized individual cannabis constituents.[14]
Putative receptor targets
The table highlights several common cannabinoids along with putative receptor targets and therapeutic properties. Exogenous (plant-derived) phytocannabinoids are identified with an asterisk while remaining chemicals represent well-known endocannabinoids (i.e., endogenously produced cannabinoid receptor ligands).
| Full Name | Known Receptor Targets | Putative Therapeutic Properties |
|---|---|---|
| Cannabichromene (CBC) | ||
| Cannabidiol (CBD) |
|
|
| Cannabigerol (CBG) | ||
| Cannabinol (CBN) |
| |
| Tetrahydrocannabinol (THC) / Delta-9-Tetrahydrocannabinol (Δ9-THC) |
|
|
| 2-Arachidonoylglycerol (2-AG) | ||
| Anandamide (AEA) | Anti-oxidative properties[16] |
Neurotransmitter interactions

In the brain, the canonical mechanism of CB1 receptor activation is a form of short-term synaptic plasticity initiated via retrograde signaling of endogenous CB1 agonists such as 2AG or AEA (two primary endocannabinoids). This mechanism of action is called depolarization-induced suppression of inhibition (DSI) or depolarization-induced suppression of excitation (DSE),[18] depending on the classification of the presynaptic neuron acted upon by the retrograde messenger (see diagram at left). In the case of CB1R agonism on the presynaptic membrane of a GABAergic interneuron, activation leads to a net effect of increased activity, while the same activity on a glutamatergic neuron leads to the opposite net effect. The release of other neurotransmitters is also modulated in this way, particularly dopamine, dynorphin, oxytocin, and vasopressin.[18]
Pharmacokinetics
When administered orally, CBN demonstrates a similar metabolism to Δ9-THC, with the primary active metabolite produced through the hydrolyzation of C9 as part of first-pass metabolism in the liver. The active metabolite generated via this process is called 11-OH-CBN, which is 2x as potent as CBN, and has demonstrated activity as a weak CB2 antagonist. This metabolism starkly contrasts that of Δ9-THC in terms of potency, given that 11-OH-THC has been reported to have 10× the potency of Δ9-THC.
Due to high lipophilicity and first-pass metabolism, there is low bioavailability of CBN and other cannabinoids following oral administration. CBN metabolism is mediated in part by CYP450 isoforms 2C9 and 3A4. The metabolism of CBN may be catalyzed by UGTs (UDP-glucuronosyltransferases), with a subset of UGT isoforms (1A7, 1A8, 1A9, 1A10, 2B7) identified as potential substrates associated with CBN glucuronidation. The bioavailability of CBN following administration via inhalation (e.g., smoking or vaporizing) is approximately 40% that of intravenous administration.
A small study of six cannabis users found a highly variable half life of 32 ± 17 hours upon intravenous administration.[19] Similar to CBD, CBN is metabolized by the CYP2C9 and CYP3A4 liver enzymes and thus the half-life is sensitive to genetic factors that effect the levels of these enzymes.[20]
Chemistry
Chemical structure
This section needs additional citations for verification. (November 2023) |
Cannabinoid receptor agonists are categorized into four groups based on chemical structure. CBN, as one of the many phytocannabinoids derived from Cannabis Sativa L, is considered a classical cannabinoid. Other examples of compounds in this group include dibenzopyran derivatives such as Δ9-THC, well-known for underlying the subjective "high" experienced by cannabis users, as well as Δ8-THC, and their synthetic analogs. In contrast, endogenously produced cannabinoids (i.e., endocannabinoids), which also exert effects through CB agonism, are considered eicosanoids, distinguished by notable differences in chemical structure.
Compared to Δ9-THC, one additional aromatic ring confers CBN with a slower and more limited metabolic profile (see § CBN Formation & Metabolism). In contrast to THC, CBN has no double bond isomers nor stereoisomers. CBN can degrade into HU-345 from oxidation. In the case of oral administration of CBN, first-pass metabolism in the liver involves the addition of a hydroxyl group at C9 or C11, increasing the affinity and specificity of CBN for both CB1 and CB2 receptors (see 11-OH-CBN).
History

CBN was the first cannabinoid to be isolated from cannabis extract in the late 1800s. Specifically, it was discovered by Barlow Wood, Newton Spivey, and Easterfield in 1896.[21] In the early 1930s, CBN's structure was identified by Cahn,[22][23] marking the first development of a cannabis extract. Its structure and chemical synthesis were achieved by 1940, followed by some of the first preclinical research studies to determine the effects of individual cannabis-derived compounds in vivo.[8]
Society and culture
Legal status
CBN is not listed in the schedules set out by the United Nations' Single Convention on Narcotic Drugs from 1961 nor their Convention on Psychotropic Substances from 1971,[24] so the signatory countries to these international drug control treaties are not required by these treaties to control CBN.
United States
According to the 2018 Farm Bill,[25] extracts from the Cannabis sativa L. plant, including CBN, are legal under US federal law as long as they have a delta-9 Tetrahydrocannabinol (THC) concentration of 0.3% or less.[26][27]
Biosynthesis

This diagram represents the biosynthetic and metabolic pathways by which phytocannabinoids (e.g., CBD, THC, CBN) are created in the cannabis plant. Starting with CBG-A, the acidic forms of certain phytocannabinoids are generated via enzymatic conversion. From there, decarboxylation (i.e., catalyzed by combustion or heat) yields the most well-known metabolites present in the cannabis plant. CBN is unique in that it does not arise from a pre-existing acidic form, but rather is generated through the oxidation of THC.
CBN is unique among phytocannabinoids in that its biosynthetic pathway involves conversion directly from Δ9-THC, rather than from an acidic precursor form of CBN (e.g., Δ9-THC arises through decarboxylation of THC-A). CBN can be found in trace amounts in the Cannabis plant, found mostly in cannabis that is aged and stored, allowing for CBN formation through the oxidation of the cannabis plant's main psychoactive and intoxicating chemical, tetrahydrocannabinol (THC). This process of oxidation occurs via exposure to heat, oxygen, and/or light. Although reports are limited, CBN-A has also been measured at very low levels in the cannabis plant, thought to have formed via hydrolyzation of THC-A (see Phytocannabinoid Biosynthesis diagram, below).
References
- ^ Cannabinol from PubChem
- ^ Lide DR (2012). CRC Handbook of Chemistry and Physics. CRC Press. pp. 3–90. ISBN 978-1-43988049-4.
- ^ "Cannabinol solution, analytical standard, for drug analysis". Sigma-Aldrich. c046.
- ^ "Cannabinol" (PDF). Biotrend. Archived from the original (PDF) on May 22, 2016.
- ^ a b c Rhee MH, Vogel Z, Barg J, Bayewitch M, Levy R, Hanus L, et al. (September 1997). "Cannabinol derivatives: binding to cannabinoid receptors and inhibition of adenylylcyclase". Journal of Medicinal Chemistry. 40 (20): 3228–3233. doi:10.1021/jm970126f. PMID 9379442.
- ^ a b c d Abood ME, Pertwee RG (2005). Cannabinoids. Berlin: Springer. ISBN 3-540-22565-X. OCLC 65169431.
- ^ Corroon J (October 2021). "Cannabinol and Sleep: Separating Fact from Fiction". Cannabis and Cannabinoid Research. 6 (5): 366–371. doi:10.1089/can.2021.0006. PMC 8612407. PMID 34468204.
- ^ a b c Pertwee RG (January 2006). "Cannabinoid pharmacology: the first 66 years". British Journal of Pharmacology. 147 (Suppl 1): S163–S171. doi:10.1038/sj.bjp.0706406. PMC 1760722. PMID 16402100.
- ^ Andre CM, Hausman JF, Guerriero G (February 4, 2016). "Cannabis sativa: The Plant of the Thousand and One Molecules". Frontiers in Plant Science. 7: 19. doi:10.3389/fpls.2016.00019. PMC 4740396. PMID 26870049.
- ^ Aizpurua-Olaizola O, Elezgarai I, Rico-Barrio I, Zarandona I, Etxebarria N, Usobiaga A (January 2017). "Targeting the endocannabinoid system: future therapeutic strategies". Drug Discovery Today. 22 (1): 105–110. doi:10.1016/j.drudis.2016.08.005. PMID 27554802. S2CID 3460960.
- ^ "Cannabinol (Code C84510)". NCI Thesaurus. National Cancer Institute, National Institutes of Health, U.S. Department of Health and Human Services.
- ^ Pattnaik F, Nanda S, Mohanty S, Dalai AK, Kumar V, Ponnusamy SK, et al. (February 2022). "Cannabis: Chemistry, extraction and therapeutic applications". Chemosphere. 289 133012. Bibcode:2022Chmsp.28933012P. doi:10.1016/j.chemosphere.2021.133012. PMID 34838836. S2CID 244679123.
- ^ a b c d e f g h i j k l m n o p q r s t u v w x y z aa ab ac Muller C, Morales P, Reggio PH (January 15, 2019). "Cannabinoid Ligands Targeting TRP Channels". Frontiers in Molecular Neuroscience. 11: 487. doi:10.3389/fnmol.2018.00487. PMC 6340993. PMID 30697147.
- ^ a b c d e Legare CA, Raup-Konsavage WM, Vrana KE (2022). "Therapeutic Potential of Cannabis, Cannabidiol, and Cannabinoid-Based Pharmaceuticals". Pharmacology. 107 (3–4): 131–149. doi:10.1159/000521683. PMID 35093949.
- ^ a b c d e f g h i j k l m n o p q r Sampson PB (January 2021). "Phytocannabinoid Pharmacology: Medicinal Properties of Cannabis sativa Constituents Aside from the "Big Two"". Journal of Natural Products. 84 (1): 142–160. doi:10.1021/acs.jnatprod.0c00965. PMID 33356248. S2CID 229694293.
- ^ a b c d e f g h i j k l m n o p q Cherkasova V, Wang B, Gerasymchuk M, Fiselier A, Kovalchuk O, Kovalchuk I (October 2022). "Use of Cannabis and Cannabinoids for Treatment of Cancer". Cancers. 14 (20): 5142. doi:10.3390/cancers14205142. PMC 9600568. PMID 36291926.
- ^ a b Mead A (June 14, 2019). "Legal and Regulatory Issues Governing Cannabis and Cannabis-Derived Products in the United States". Frontiers in Plant Science. 10: 697. doi:10.3389/fpls.2019.00697. PMC 6590107. PMID 31263468.
- ^ a b Diana MA, Marty A (May 2004). "Endocannabinoid-mediated short-term synaptic plasticity: depolarization-induced suppression of inhibition (DSI) and depolarization-induced suppression of excitation (DSE)". British Journal of Pharmacology. 142 (1): 9–19. doi:10.1038/sj.bjp.0705726. PMC 1574919. PMID 15100161.
- ^ Johansson E, Ohlsson A, Lindgren JE, Agurell S, Gillespie H, Hollister LE (September 1987). "Single-dose kinetics of deuterium-labelled cannabinol in man after intravenous administration and smoking". Biomedical & Environmental Mass Spectrometry. 14 (9): 495–499. doi:10.1002/bms.1200140904. PMID 2960395.
- ^ Stout SM, Cimino NM (February 2014). "Exogenous cannabinoids as substrates, inhibitors, and inducers of human drug metabolizing enzymes: a systematic review". Drug Metabolism Reviews. 46 (1): 86–95. doi:10.3109/03602532.2013.849268. PMID 24160757. S2CID 29133059.
- ^ Wood TB, Spivey WN, Easterfield III TH (1899). "III.—Cannabinol. Part I". Journal of the Chemical Society, Transactions. 75: 20–36. doi:10.1039/CT8997500020.
- ^ Cahn RS (1932). "174. Cannabis indica resin. Part III. The constitution of cannabinol". Journal of the Chemical Society (Resumed): 1342–1353. doi:10.1039/JR9320001342.
- ^ Pertwee RG (January 2006). "Cannabinoid pharmacology: the first 66 years". British Journal of Pharmacology. 147 (Suppl 1): S163–S171. doi:10.1038/sj.bjp.0706406. PMC 1760722. PMID 16402100.
- ^ "UN International Drug Control Conventions". United Nations Office on Drugs and Crime. United Nations Commission on Narcotic Drugs. Archived from the original on March 17, 2014. Retrieved February 15, 2017.
- ^ Office of the Commissioner (October 18, 2021). "FDA Regulation of Cannabis and Cannabis-Derived Products, Including Cannabidiol (CBD)". FDA. Archived from the original on October 1, 2019.
- ^ Mead A (May 2017). "The legal status of cannabis (marijuana) and cannabidiol (CBD) under U.S. law". Epilepsy & Behavior. 70 (Pt B): 288–291. doi:10.1016/j.yebeh.2016.11.021. PMID 28169144.
- ^ "Section 1308.11 Schedule I". Code of Federal Regulations. Office of Diversion Control, Drug Enforcement Administration, U.S. Department of Justice. Archived from the original on February 9, 2012.
External links
- Erowid Compounds found in Cannabis sativa
Notes
This article is a direct transclusion of the Wikipedia article and therefore may not meet the same editing standards as LIMSwiki.









