Difference between revisions of "User:Shawndouglas/sandbox/sublevel32"
Shawndouglas (talk | contribs) |
Shawndouglas (talk | contribs) |
||
| Line 1: | Line 1: | ||
==1. Overview of COVID-19 and its challenges== | ==1. Overview of COVID-19 and its challenges== | ||
''Please note | ''Please note'': Information during a pandemic changes, sometime rapidly, in regards to test methods, reported figures, and social situations. Efforts will be made to keep this guide up-to-date as best as possible given time constraints and resources. | ||
===1.1 COVID-19: The terminology=== | ===1.1 COVID-19: The terminology=== | ||
| Line 41: | Line 41: | ||
* ''Understanding of high viral loads and infectious doses'': Respiratory diseases such as influenza, SARS, and MERS see a correlation between the infectious dose amount and the severity of disease symptoms, meaning the higher the infectious dose, the worse the symptoms.<ref name="GeddesDoesA20">{{cite web |url=https://www.newscientist.com/article/2238819-does-a-high-viral-load-or-infectious-dose-make-covid-19-worse/ |title=Does a high viral load or infectious dose make covid-19 worse? |author=Geddes, L. |work=New Scientist |date=27 March 2020 |accessdate=01 April 2020}}</ref> Similarly, viral load—a quantification of viral genomic fragments—also tends to correlate with clinical symptoms.<ref name="HijanoClinical19">{{cite journal |title=Clinical correlation of influenza and respiratory syncytial virus load measured by digital PCR |journal=PLoS One |author=Hijano, D.R.; Brazelton de Cardenas, J.; Maron, G. et al. |volume=14 |issue=9 |at=e0220908 |year=2019 |doi=10.1371/journal.pone.0220908 |pmid=31479459 |pmc=PMC6720028}}</ref> However, we are still in the investigative stages of determining if that similarly holds true to COVID-19.<ref name="GeddesDoesA20" /><ref name="LiuViral20">{{cite journal |title=Viral dynamics in mild and severe cases of COVID-19 |journal=The Lancet Infectious Diseases |author=Liu, Y.; Yan, L.-M.; Wan, L. et al. |year=2020 |doi=10.1016/S1473-3099(20)30232-2 |pmid=32199493}}</ref><ref name="JoyntUnder20">{{cite journal |title=Understanding COVID-19: what does viral RNA load really mean? |journal=The Lancet Infectious Diseases |author=Joynt, G.M.; Wu, W.K.K. |year=2020 |doi=10.1016/S1473-3099(20)30237-1}}</ref> Early research seem to indicate, for example, there is little difference between the viral load of those with mild or no COVID-19 symptoms and those with more severe symptoms.<ref name="GeddesDoesA20" /> More research must be performed to better understand how the viral load infectious dose plays a role in transmission. Given these unknowns, social distancing, wearing masks, and other means of minimizing exposure remain the best defense against the disease.<ref name="GeddesDoesA20" /> | * ''Understanding of high viral loads and infectious doses'': Respiratory diseases such as influenza, SARS, and MERS see a correlation between the infectious dose amount and the severity of disease symptoms, meaning the higher the infectious dose, the worse the symptoms.<ref name="GeddesDoesA20">{{cite web |url=https://www.newscientist.com/article/2238819-does-a-high-viral-load-or-infectious-dose-make-covid-19-worse/ |title=Does a high viral load or infectious dose make covid-19 worse? |author=Geddes, L. |work=New Scientist |date=27 March 2020 |accessdate=01 April 2020}}</ref> Similarly, viral load—a quantification of viral genomic fragments—also tends to correlate with clinical symptoms.<ref name="HijanoClinical19">{{cite journal |title=Clinical correlation of influenza and respiratory syncytial virus load measured by digital PCR |journal=PLoS One |author=Hijano, D.R.; Brazelton de Cardenas, J.; Maron, G. et al. |volume=14 |issue=9 |at=e0220908 |year=2019 |doi=10.1371/journal.pone.0220908 |pmid=31479459 |pmc=PMC6720028}}</ref> However, we are still in the investigative stages of determining if that similarly holds true to COVID-19.<ref name="GeddesDoesA20" /><ref name="LiuViral20">{{cite journal |title=Viral dynamics in mild and severe cases of COVID-19 |journal=The Lancet Infectious Diseases |author=Liu, Y.; Yan, L.-M.; Wan, L. et al. |year=2020 |doi=10.1016/S1473-3099(20)30232-2 |pmid=32199493}}</ref><ref name="JoyntUnder20">{{cite journal |title=Understanding COVID-19: what does viral RNA load really mean? |journal=The Lancet Infectious Diseases |author=Joynt, G.M.; Wu, W.K.K. |year=2020 |doi=10.1016/S1473-3099(20)30237-1}}</ref> Early research seem to indicate, for example, there is little difference between the viral load of those with mild or no COVID-19 symptoms and those with more severe symptoms.<ref name="GeddesDoesA20" /> More research must be performed to better understand how the viral load infectious dose plays a role in transmission. Given these unknowns, social distancing, wearing masks, and other means of minimizing exposure remain the best defense against the disease.<ref name="GeddesDoesA20" /> | ||
* ''Cardiovascular issues'': Coronaviruses and their accompanying respiratory infections are known to complicate issues of the cardiovascular system, which in turn may "increase the incidence and severity" of infectious diseases such as SARS and COVID-19.<ref name="MadjidPotent20">{{cite journal |title=Potential Effects of Coronaviruses on the Cardiovascular System |journal=JAMA Cardiology |author=Madjid, M.; Safavi-Naeini, P.; Solomon, S.D. |year=2020 |doi=10.1001/jamacardio.2020.1286 |pmid=32219363}}</ref><ref name="XiongCorona20">{{cite journal |title=Coronaviruses and the cardiovascular system: acute and long-term implications |journal=European Heart Journal |author=Xiong, T.-Y.; Redwood, S.; Prendergast, B.; Chen, M. |at=ehaa231 |year=2020 |doi=10.1093/eurheartj/ehaa231 |pmid=32186331}}</ref><ref name="DrigginCardio20">{{cite journal |title=Cardiovascular Considerations for Patients, Health Care Workers, and Health Systems During the Coronavirus Disease 2019 (COVID-19) Pandemic |journal=Journal of the American College of Cardiology |author=Driggin, E.; Madhavan, M.V.; Bikdeli, B. et al. |year=2020 |doi=10.1016/j.jacc.2020.03.031 |pmid=32201335}}</ref> While the exact cardiac effect COVID-19 has on patients is still unknown, suspicion is those with "hypertension, diabetes, and diagnosed cardiovascular disease" may be more prone to having cardiovascular complications from the disease.<ref name="OttoCardiac20">{{cite web |url=https://www.the-hospitalist.org/hospitalist/article/219645/coronavirus-updates/cardiac-symptoms-can-be-first-sign-covid-19 |title=Cardiac symptoms can be first sign of COVID-19 |author=Otto, M.A. |work=The Hospitalist |date=26 March 2020 |accessdate=01 April 2020}}</ref><ref name="ClerkinCorona20">{{cite journal |title=Coronavirus Disease 2019 (COVID-19) and Cardiovascular Disease |journal=Circulation |author=Clerkin, K.J.; Fried, J.A.; Raikhelkar, J. et al. |year=2020 |doi=10.1161/CIRCULATIONAHA.120.046941 |pmid=32200663}}</ref> Current thinking is SARS-CoV-2 either attacks heart tissues, causing myocardial dysfunction, or inevitably causes heart failure through a "cytokine storm,"<ref name="MadjidPotent20" /><ref name="XiongCorona20" /><ref name="OttoCardiac20" /><ref name="ClerkinCorona20" /><ref name="MehtaCOVID20">{{cite journal |title=COVID-19: Consider cytokine storm syndromes and immunosuppression |journal=The Lancet |author=Mehta, P.; McAuley, D.F.; Brown, M. et al. |volume=395 |issue=10229 |pages=P1033–34 |year=2020 |doi=10.1016/S0140-6736(20)30628-0 |pmid=32192578}}</ref><ref name="MandavilliTheCoronaCyto20">{{cite web |url=https://www.nytimes.com/2020/04/01/health/coronavirus-cytokine-storm-immune-system.html |title=The Coronavirus Patients Betrayed by Their Own Immune Systems |author=Mandavilli, A. |work=The New York Times |date=01 April 2020 |accessdate=01 April 2020}}</ref>, an overproduction of signaling molecules that promote inflammation by white blood cells (leukocytes).<ref name="TisoncikInto12">{{cite journal |title=Into the eye of the cytokine storm |journal=Microbiology and Molecular Biology Reviews |author=Tisoncik, J.R.; Korth, M.J.; Simmons, C.P. et al. |volume=76 |issue=1 |pages=16–32 |year=2012 |doi=10.1128/MMBR.05015-11 |pmid=22390970 |pmc=PMC3294426}}</ref> What's scary is that like the 1918 Spanish flu, SARS, and other epidemics, some otherwise healthy patients' immune responses are entirely overreactive, leading to acute respiratory distress syndrome (ARDS) or heart failure.<ref name="MandavilliTheCoronaCyto20" /><ref name="BasilioANew20">{{cite web |url=https://www.mdlinx.com/internal-medicine/article/6590 |title=A new potential risk of COVID-19: Sudden cardiac death |author=Basilio, P. |work=MDLinx |date=26 March 2020 |accessdate=01 April 2020}}</ref> Additionally, as the disease has progressed, medical professionals have noted abnormal amounts of blood clotting in infected patients, which may or may not be related to overreactive immune systems and underlying health conditions.<ref name="RettnerMyster20">{{cite web |url=https://www.livescience.com/coronavirus-blood-clots.html |title=Mysterious blood clots in COVID-19 patients have doctors alarmed |author=Rettner, R. |work=LiveScience |date=23 April 2020 |accessdate=28 April 2020}}</ref> These uncertainties only add to the level of difficulty of properly treating COVID-19. | * ''Cardiovascular issues'': Coronaviruses and their accompanying respiratory infections are known to complicate issues of the cardiovascular system, which in turn may "increase the incidence and severity" of infectious diseases such as SARS and COVID-19.<ref name="MadjidPotent20">{{cite journal |title=Potential Effects of Coronaviruses on the Cardiovascular System |journal=JAMA Cardiology |author=Madjid, M.; Safavi-Naeini, P.; Solomon, S.D. |year=2020 |doi=10.1001/jamacardio.2020.1286 |pmid=32219363}}</ref><ref name="XiongCorona20">{{cite journal |title=Coronaviruses and the cardiovascular system: acute and long-term implications |journal=European Heart Journal |author=Xiong, T.-Y.; Redwood, S.; Prendergast, B.; Chen, M. |at=ehaa231 |year=2020 |doi=10.1093/eurheartj/ehaa231 |pmid=32186331}}</ref><ref name="DrigginCardio20">{{cite journal |title=Cardiovascular Considerations for Patients, Health Care Workers, and Health Systems During the Coronavirus Disease 2019 (COVID-19) Pandemic |journal=Journal of the American College of Cardiology |author=Driggin, E.; Madhavan, M.V.; Bikdeli, B. et al. |year=2020 |doi=10.1016/j.jacc.2020.03.031 |pmid=32201335}}</ref> While the exact cardiac effect COVID-19 has on patients is still unknown, suspicion is those with "hypertension, diabetes, and diagnosed cardiovascular disease" may be more prone to having cardiovascular complications from the disease.<ref name="OttoCardiac20">{{cite web |url=https://www.the-hospitalist.org/hospitalist/article/219645/coronavirus-updates/cardiac-symptoms-can-be-first-sign-covid-19 |title=Cardiac symptoms can be first sign of COVID-19 |author=Otto, M.A. |work=The Hospitalist |date=26 March 2020 |accessdate=01 April 2020}}</ref><ref name="ClerkinCorona20">{{cite journal |title=Coronavirus Disease 2019 (COVID-19) and Cardiovascular Disease |journal=Circulation |author=Clerkin, K.J.; Fried, J.A.; Raikhelkar, J. et al. |year=2020 |doi=10.1161/CIRCULATIONAHA.120.046941 |pmid=32200663}}</ref> Current thinking is SARS-CoV-2 either attacks heart tissues, causing myocardial dysfunction, or inevitably causes heart failure through a "cytokine storm,"<ref name="MadjidPotent20" /><ref name="XiongCorona20" /><ref name="OttoCardiac20" /><ref name="ClerkinCorona20" /><ref name="MehtaCOVID20">{{cite journal |title=COVID-19: Consider cytokine storm syndromes and immunosuppression |journal=The Lancet |author=Mehta, P.; McAuley, D.F.; Brown, M. et al. |volume=395 |issue=10229 |pages=P1033–34 |year=2020 |doi=10.1016/S0140-6736(20)30628-0 |pmid=32192578}}</ref><ref name="MandavilliTheCoronaCyto20">{{cite web |url=https://www.nytimes.com/2020/04/01/health/coronavirus-cytokine-storm-immune-system.html |title=The Coronavirus Patients Betrayed by Their Own Immune Systems |author=Mandavilli, A. |work=The New York Times |date=01 April 2020 |accessdate=01 April 2020}}</ref>, an overproduction of signaling molecules that promote inflammation by white blood cells (leukocytes).<ref name="TisoncikInto12">{{cite journal |title=Into the eye of the cytokine storm |journal=Microbiology and Molecular Biology Reviews |author=Tisoncik, J.R.; Korth, M.J.; Simmons, C.P. et al. |volume=76 |issue=1 |pages=16–32 |year=2012 |doi=10.1128/MMBR.05015-11 |pmid=22390970 |pmc=PMC3294426}}</ref> What's scary is that like the 1918 Spanish flu, SARS, and other epidemics, some otherwise healthy patients' immune responses are entirely overreactive, leading to acute respiratory distress syndrome (ARDS) or heart failure.<ref name="MandavilliTheCoronaCyto20" /><ref name="BasilioANew20">{{cite web |url=https://www.mdlinx.com/internal-medicine/article/6590 |title=A new potential risk of COVID-19: Sudden cardiac death |author=Basilio, P. |work=MDLinx |date=26 March 2020 |accessdate=01 April 2020}}</ref> Additionally, as the disease has progressed, medical professionals have noted abnormal amounts of blood clotting in infected patients, which may or may not be related to overreactive immune systems and underlying health conditions.<ref name="RettnerMyster20">{{cite web |url=https://www.livescience.com/coronavirus-blood-clots.html |title=Mysterious blood clots in COVID-19 patients have doctors alarmed |author=Rettner, R. |work=LiveScience |date=23 April 2020 |accessdate=28 April 2020}}</ref> These uncertainties only add to the level of difficulty of properly treating COVID-19. | ||
==References== | ==References== | ||
{{Reflist|colwidth=30em}} | {{Reflist|colwidth=30em}} | ||
Revision as of 21:11, 1 May 2020
1. Overview of COVID-19 and its challenges
Please note: Information during a pandemic changes, sometime rapidly, in regards to test methods, reported figures, and social situations. Efforts will be made to keep this guide up-to-date as best as possible given time constraints and resources.
1.1 COVID-19: The terminology
A pneumonia-like outbreak was fully in process in Wuhan—located in the Hubei province of China—by December 2019. The World Health Organization (WHO) was notified by the end of the month that the cause could be a novel threat to the larger populace.[1] By the end of January, the WHO had declared the growing viral threat a Public Health Emergency of International Concern (PHEIC), an act which includes with it a need "to implement a comprehensive risk communication strategy."[2] As the disease progressed beyond its Chinese origins, public confusion slowly grew regarding the terminology surrounding the disease. Leaders at the WHO and the Coronavirus Study Group (CSG) of the International Committee on Taxonomy of Viruses came to different naming conclusions, differing in their naming conventions while adding to the confusion.[3][4] In the end, "COVID-19" has ended up as the common disease name, caused by the SARS-CoV-2 virus, which is a member of the coronavirus family. Today, however, some still refer to the disease simply as "coronavirus," which is in error.
This isn't the first time a disease has had a different name from its associated virus. One should look back to 1982, when the U.S. Centers for Disease Control and Prevention (CDC) gave the name "acquired immune deficiency syndrome" or "AIDS" to the disease associated with the human immunodeficiency virus (HIV) (a member of the retrovirus family).[5] It took time for the layman to get used to the terminology, and even then some still ended up mistakenly referring to the disease as "HIV."
Consistent terminology is vital to communicating technical material to a global audience.[6][7] With that in mind, it's beneficial to ensure everyone is clear on the terms used. For purposes of this guide:
- Coronavirus disease 2019 (otherwise known as COVID-19) is the respiratory disease being discussed in this guide.
- SARS-CoV-2 is the virus responsible for COVID-19.
- Coronavirus (or Coronaviridae) is a family of related viruses, of which SARS-CoV-2 is a member.
- Severe acute respiratory syndrome (otherwise known as SARS) is a different respiratory disease, which surfaced in the early 2000s, caused by a related but different type of coronavirus (SARS-CoV or SARS-CoV-1).
- Middle East respiratory syndrome (otherwise known as MERS) is a different respiratory disease, which surfaced in 2012, caused by a related but different type of coronavirus (MERS-CoV).
1.2 COVID-19: History and impact (so far)
COVID-19 is an infectious disease caused by the SARS-CoV-2 virus, typically yielding symptoms of fever, cough, shortness of breath, and loss of taste or smell.[8] A majority of cases yield relatively mild symptoms, but some progress to life-threatening situations involving pneumonia, organ failure, and cardiovascular complication.[9][10]
The first known case of COVID-19 dates back to November 2019, "according to government data seen by the South China Morning Post."[11] By the middle of December, infections were at 27, and by the end of the year the number was 266.[11] By that time, Chinese health authorities had been updated that the pneumonia-like symptoms of patients in China's Hubei province may have been the symptoms of a disease caused by a novel (new) coronavirus[11], and the WHO was notified.[1] At the start of 2020, that number grew to 381 known cases[11], jumping to more than 7,700 confirmed and 12,000 suspected cases by the end of January.[2] By that time, the WHO had convened a second meeting of its Emergency Committee to discuss the declaration of a PHEIC, saying the then-called "2019-nCoV" constituted a health emergency of international concern.[2] This spurred the publishing of WHO technical advice to other countries, with a focus on "reducing human infection, prevention of secondary transmission and international spread, and contributing to the international response."[2] However, at the same time, the virus was already beginning to spread in locations such as Australia[12], France[13], Germany[14] Italy[15], Japan[16], South Korea[17], Spain[18], the United Kingdom[19], and the United States.[20]
As the disease continued to spread in February, naming conventions came together, with the WHO declaring the disease's name "COVID-19," short for "coronavirus disease 2019."[3][4] By the end of the month, the WHO warned a "very high" likelihood the virus's spread could turn into a full pandemic.[21] Less than two weeks later, on March 11, 2020, the WHO declared the outbreak of SARS-CoV-2 a pandemic, noting more than 118,000 confirmed cases and 4,000 deaths on all continents except Antarctica.[22] As of April 28, the number of confirmed cases was nearly three million, with more than 200,000 people dead.[23]
Governmental reaction to the pandemic around the globe has varied significantly since the pandemic's declaration in March. Some of that variance can be seen when reviewing the various policies implemented by the world's governments. The International Monetary Fund's policy tracker for COVID-19 response, for example, paints a picture of the laboratory testing, social, transportation, trade, and financial situations of each country. Reviewing it shows that Kosovo, for example, has implemented citizen lockdowns, not allowing people to leave their homes for more than 1.5 hours per day. Other more comprehensive measures such as widespread testing and digital tracking, with fewer mobility restrictions, have allowed South Korea to virtually have their daily reported case numbers shrink to less than 15. After strict stay-at-home rules, complete with enforcement, Austria has been able to gradually reopen its operations as of mid-April while also supporting citizens through debt servicing delays, financial aid for the self-employed and micro-businesses, and prohibitions on banks from share buy-back.[24] Another source for examining government reaction is through the collation of data on how governments have implemented technological tracking measures in the name of slowing the epidemic. Groups like Privacy International collate such information through their collective tracking project, which links to hundreds of news stories concerning the forced sharing of mobile phone data, the use of drones and other surveillance for tracking and enforcing quarantines, geolocation tracking though phones, and the implementation of facial recognition technology.[25] The U.S. Chamber of Commerce also collects a dashboard of governmental policies for comparison.[26]
Citizen reaction to the pandemic has also varied. Local governments in China have been criticized[27][28], while the central government has, at least at times, been seen in positive light for its handling of the pandemic.[29][30][31] Some Indians have criticized their government for its police brutality during lockdowns[32], while some Italians have criticized their government for trivializing the situation for too long.[33] In the U.S.—and in other parts of the world—criticism has been rampant concerning the United States government's response[34][35][36][37], though some governors have received praise for standing up for their state's citizens.[38][39][40]
It's too early to truly quantitatively (or qualitatively) measure the impact of COVID-19 on the world, let alone the United States. But the effects of the virus are taking shape, from significant job losses[41] and bankruptcies[42], to poor mental health impacts[43] and postponed cancer surgeries.[44] What has long been known and remains true, however, is that beyond preventative measures, in order to further limit the negative consequences of the pandemic, testing must be expanded.[45][46]
1.3 Challenges of managing the disease in the human population
COVID-19 has presented numerous societal challenges, from supply line interruptions and economic sagging to overwhelmed healthcare systems and civil disorder. However, these are largely the social, economic, and political ripple effects of a disease that has brought with it a set of inherent attributes that make it more difficult to manage in human populations than say the flu.
However, COVID-19 is not the flu, and it is indeed worse in its effects than the flu, contrary to many people's perceptions. Yes, COVID-19 and the flu have some symptom overlap. Yes, COVID-19 and the flu have some transmission type overlap. But from there it diverges. COVID-19 is different in that it is more prone to be transmitted to others during the presymptomatic phase. The disease may also be transmittable in other ways, such as an airborne route, though research is ongoing.[47] Hospitalization rates are higher, perhaps up to 10 times higher than the flu, and hospital stays are longer with COVID-19. People are dying more often from COVID-19 too, up to 10 times more often than people stricken with the flu. And of course, whereas people have been acquiring the flu vaccine yearly, limiting the percentage of the population that becomes ill, there is yet no vaccine for COVID-19, meaning everyone is susceptible.[48][49][50]
Other aspects of the disease that make this difficult to manage include:
- Median incubation period: According to research published in Annals of Internal Medicine, the median (i.e., the central tendency, which is less skewed than average[51]) incubation period is 5.1 days, with 97.5% of symptomatic carriers showing symptoms within 11.5 days. The authors found this to be compatible with U.S. government recommendations of monitored 14-day self-quarantines if individuals were at risk of exposure.[52] However, many people continue to not take self-quarantines and other forms of social distancing seriously[53][54][55][56], and presymptomatic (and asymptomatic) carriers are thus more prone to spreading the virus.[57][58]
- Presymptomatic and asymptomatic virus shedding: As mentioned in the previous point, carriers can be contagious during the presymptomatic phase of the disease, even while remaining symptom-free.[57][58][59][60] This contagion is a result of what's called viral shedding, when the virus moves from cell to cell following successful reproduction. When the virus is in this state, it can be actively found in a carrier's body fluids, excrement, and other sources. Depending on the virus, the virus can then be introduced to another person via those sources. In the case of COVID-19, the route of transmission is still being studied[61][62], though water droplets (from sneezes, cough, talking, etc.) and potentially even aerosolized water droplets (water droplets from the body that have become fine spray or suspension in the air) are likely sources.[62] This initial uncertainty of transmission routes, along with mixed messages early on about masks and their effectiveness for COVID-19[62][63][64], makes social distancing an even stronger necessity to limit community transmission of the disease.
- Understanding of high viral loads and infectious doses: Respiratory diseases such as influenza, SARS, and MERS see a correlation between the infectious dose amount and the severity of disease symptoms, meaning the higher the infectious dose, the worse the symptoms.[65] Similarly, viral load—a quantification of viral genomic fragments—also tends to correlate with clinical symptoms.[66] However, we are still in the investigative stages of determining if that similarly holds true to COVID-19.[65][67][68] Early research seem to indicate, for example, there is little difference between the viral load of those with mild or no COVID-19 symptoms and those with more severe symptoms.[65] More research must be performed to better understand how the viral load infectious dose plays a role in transmission. Given these unknowns, social distancing, wearing masks, and other means of minimizing exposure remain the best defense against the disease.[65]
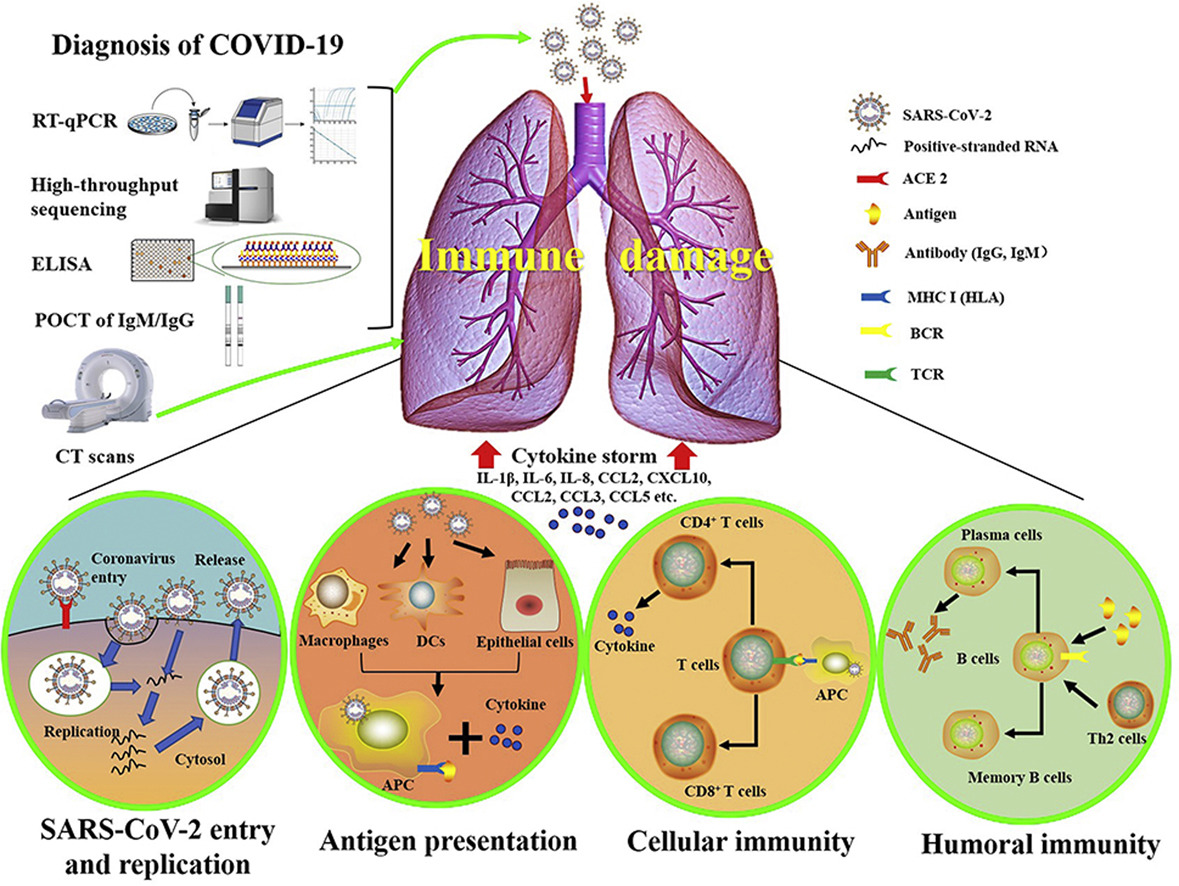
- Cardiovascular issues: Coronaviruses and their accompanying respiratory infections are known to complicate issues of the cardiovascular system, which in turn may "increase the incidence and severity" of infectious diseases such as SARS and COVID-19.[69][70][71] While the exact cardiac effect COVID-19 has on patients is still unknown, suspicion is those with "hypertension, diabetes, and diagnosed cardiovascular disease" may be more prone to having cardiovascular complications from the disease.[72][73] Current thinking is SARS-CoV-2 either attacks heart tissues, causing myocardial dysfunction, or inevitably causes heart failure through a "cytokine storm,"[69][70][72][73][74][75], an overproduction of signaling molecules that promote inflammation by white blood cells (leukocytes).[76] What's scary is that like the 1918 Spanish flu, SARS, and other epidemics, some otherwise healthy patients' immune responses are entirely overreactive, leading to acute respiratory distress syndrome (ARDS) or heart failure.[75][77] Additionally, as the disease has progressed, medical professionals have noted abnormal amounts of blood clotting in infected patients, which may or may not be related to overreactive immune systems and underlying health conditions.[78] These uncertainties only add to the level of difficulty of properly treating COVID-19.
References
- ↑ 1.0 1.1 Hui, D.S.; Azhar, E.I.; Madani, T.A. et al. (2020). "The continuing 2019-nCoV epidemic threat of novel coronaviruses to global health—The latest 2019 novel coronavirus outbreak in Wuhan, China". International Journal of Infectious Diseases 91: 264–66. doi:10.1016/j.ijid.2020.01.009. PMID 31953166.
- ↑ 2.0 2.1 2.2 2.3 World Health Organization (30 January 2020). "Statement on the second meeting of the International Health Regulations (2005) Emergency Committee regarding the outbreak of novel coronavirus (2019-nCoV)". World Health Organization. https://www.who.int/news-room/detail/30-01-2020-statement-on-the-second-meeting-of-the-international-health-regulations-(2005)-emergency-committee-regarding-the-outbreak-of-novel-coronavirus-(2019-ncov). Retrieved 31 March 2020.
- ↑ 3.0 3.1 Enserink, M. (12 February 2020). "Update: ‘A bit chaotic.’ Christening of new coronavirus and its disease name create confusion". Science. https://www.sciencemag.org/news/2020/02/bit-chaotic-christening-new-coronavirus-and-its-disease-name-create-confusion. Retrieved 30 March 2020.
- ↑ 4.0 4.1 Jiang, S.; Shi, Z.; Shu, Y. et al. (2020). "A distinct name is needed for the new coronavirus". The Lancet 395 (10228): 949. doi:10.1016/S0140-6736(20)30419-0. PMID 32087125.
- ↑ Oppenheimer, G.M. (1992). "Chapter 2: Causes, Cases, and Cohorts: The Role of Epidemiology in the Historical Construction of AIDS". In Fee, E.; Fox, D.M.. AIDS: The Making of a Chronic Disease. University of California Press. pp. 49–83. ISBN 0520077784. https://books.google.com/books?id=CmME6xfdEFAC&pg=PA49. Retrieved 31 March 2020.
- ↑ Kohl, J.R. (2008). The Global English Style Guide: Writing Clear, Trnaslatable Documentation for a Global Market. SAS Institute. ISBN 9781599946573.
- ↑ Megathlin, B.A.; Langford, R.S. (1991). "Controlling the Unruly: Terminology". 1991 Proceedings 38th International Technical Communication Conference: WE22–WE24.
- ↑ Centers for Disease Control and Preventions (20 March 2020). "Symptoms of Coronavirus". Centers for Disease Control and Preventions. https://www.cdc.gov/coronavirus/2019-ncov/symptoms-testing/symptoms.html. Retrieved 01 May 2020.
- ↑ Wadman, M.; Couzin-Frankel, J.; Kaiser, J. et al. (17 April 2020). "How does coronavirus kill? Clinicians trace a ferocious rampage through the body, from brain to toes". Science. doi:10.1126/science.abc3208. https://www.sciencemag.org/news/2020/04/how-does-coronavirus-kill-clinicians-trace-ferocious-rampage-through-body-brain-toes. Retrieved 01 May 2020.
- ↑ Chinese Center for Disease Control and Prevention (2020). "The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19) in China". Chinese Journal of Epidemiology 41 (2): 145–51. doi:10.3760/cma.j.issn.0254-6450.2020.02.003. PMID 32064853.
- ↑ 11.0 11.1 11.2 11.3 Ma, J. (13 March 2020). "Coronavirus: China’s first confirmed Covid-19 case traced back to November 17". South China Morning Post. https://www.scmp.com/news/china/society/article/3074991/coronavirus-chinas-first-confirmed-covid-19-case-traced-back. Retrieved 31 March 2020.
- ↑ Hunt, G. (25 January 2020). "First confirmed case of novel coronavirus in Australia". Australian Department of Health. https://www.health.gov.au/ministers/the-hon-greg-hunt-mp/media/first-confirmed-case-of-novel-coronavirus-in-australia. Retrieved 31 March 2020.
- ↑ Jacob, E. (24 January 2020). "Coronavirus: trois premiers cas confirmés en France, deux d’entre eux vont bien". Le Figaro. https://www.lefigaro.fr/sciences/coronavirus-trois-premiers-cas-confirmes-en-france-20200124. Retrieved 31 March 2020.
- ↑ Der Spiegel (28 January 2020). "Bayerische Behörden bestätigen ersten Fall in Deutschland". https://www.spiegel.de/wissenschaft/medizin/corona-virus-erster-fall-in-deutschland-bestaetigt-a-19843b8d-8694-451f-baf7-0189d3356f99. Retrieved 31 March 2020.
- ↑ Severgnini, C. (30 January 2020). "Coronavirus, primi due casi in Italia «Sono due cinesi in vacanza a Roma» Sono arrivati a Milano il 23 gennaio". Corriere della Sera. https://www.corriere.it/cronache/20_gennaio_30/coronavirus-italia-corona-9d6dc436-4343-11ea-bdc8-faf1f56f19b7.shtml. Retrieved 31 March 2020.
- ↑ Sim, W. (16 January 2020). "Japan confirms first case of infection from Wuhan coronavirus; Vietnam quarantines two tourists". The Straits Times. https://www.straitstimes.com/asia/east-asia/japan-confirms-first-case-of-infection-with-new-china-coronavirus. Retrieved 31 March 2020.
- ↑ Jin-woo, S. (24 January 2020). "신종 코로나바이러스 한국인 첫환자 확인". Maekyung.com. https://www.mk.co.kr/news/society/view/2020/01/80017/. Retrieved 31 March 2020.
- ↑ Linde, P. (31 January 2020). "Sanidad confirma en La Gomera el primer caso de coronavirus en España". El País. https://elpais.com/sociedad/2020/01/31/actualidad/1580509404_469734.html. Retrieved 31 March 2020.
- ↑ Ball, T.; Wace, C. (31 January 2020). "Hunt for contacts of coronavirus-stricken pair in York". The Times. https://www.thetimes.co.uk/article/hunt-for-contacts-of-coronavirus-stricken-pair-in-york-dh363qf8k. Retrieved 31 March 2020.
- ↑ Holshue, M.L.; DeBolt, C.; Lindquist, S. et al. (2020). "First Case of 2019 Novel Coronavirus in the United States". New England Journal of Medicine 382 (10): 929–36. doi:10.1056/NEJMoa2001191. PMID 32004427.
- ↑ Mulier, T. (28 February 2020). "WHO Raises Global Risk for Coronavirus to Very High". Bloomberg. https://www.bloomberg.com/news/articles/2020-02-28/who-raises-global-risk-for-coronavirus-to-very-high-from-high. Retrieved 31 March 2020.
- ↑ Gumbrecht, J.; Howard, J. (11 March 2020). "WHO declares novel coronavirus outbreak a pandemic". CNN Health. https://www.cnn.com/2020/03/11/health/coronavirus-pandemic-world-health-organization/index.html. Retrieved 31 March 2020.
- ↑ World Health Organization (28 April 2020). "Coronavirus disease 2019 (COVID-19) Situation Report – 99" (PDF). World Health Organization. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200428-sitrep-99-covid-19.pdf. Retrieved 28 April 2020.
- ↑ International Monetary Fund (24 April 2020). "Policy Responses to COVID-19". International Monetary Fund. https://www.imf.org/en/Topics/imf-and-covid19/Policy-Responses-to-COVID-19. Retrieved 25 April 2020.
- ↑ Privacy International (21 April 2020). "Tracking the Global Response to COVID-19". Privacy International. https://privacyinternational.org/examples/tracking-global-response-covid-19. Retrieved 25 April 2020.
- ↑ U.S. Chamber of Commerce (24 April 2020). "Global Dashboard on COVID-19 Government Policies". U.S. Chamber of Commerce. https://www.uschamber.com/international-affairs-division/covid-dashboard. Retrieved 25 April 2020.
- ↑ Wu, H.; Cheng, L. (26 January 2020). "Chinese provincial press conference on coronavirus inspires anger, criticism". Reuters. https://www.reuters.com/article/us-china-health-governor-idUSKBN1ZP0RU. Retrieved 25 April 2020.
- ↑ She, Z. (21 January 2020). "武汉"万家宴":他们的淡定让人没法淡定". The Beijing News. Archived from the original on 28 January 2020. https://web.archive.org/web/20200128221902/http://www.bjnews.com.cn/opinion/2020/01/21/677335.html. Retrieved 25 April 2020.
- ↑ Johnson, I. (13 March 2020). "China Bought the West Time. The West Squandered It". The New York Times. https://www.nytimes.com/2020/03/13/opinion/china-response-china.html. Retrieved 25 April 2020.
- ↑ Richie, R. (28 March 2020). "Rodney Richie: Don’t be quick to blame Chinese for obscuring viral contagion". Waco Tribune-Herald. https://www.wacotrib.com/opinion/columns/guest_columns/rodney-richie-don-t-be-quick-to-blame-chinese-for-obscuring-viral-contagion/article_91f410f5-07a9-549a-9f8c-8b785bfc1207.html. Retrieved 25 April 2020.
- ↑ Bowman, N. (18 March 2020). "Bill Gates estimates at least 6-10 weeks before coronavirus is quelled in US". MYNorthwest. https://mynorthwest.com/1773883/bill-gates-coronavirus-reddit-ama/. Retrieved 25 April 2020.
- ↑ PTI (27 March 2020). "Coronavirus: Bollywood celebrities criticise police brutality during lockdown". Deccan Herald. https://www.deccanherald.com/national/coronavirus-bollywood-celebrities-criticise-police-brutality-during-lockdown-818202.html. Retrieved 25 April 2020.
- ↑ Horowitz, J.; Bubola, E.; Povoledo, E. (21 March 2020). "Italy, Pandemic’s New Epicenter, Has Lessons for the World". The New York Times. https://www.nytimes.com/2020/03/21/world/europe/italy-coronavirus-center-lessons.html. Retrieved 25 April 2020.
- ↑ Science News Staff (1 April 2020). "The United States leads in coronavirus cases, but not pandemic response". Science. https://www.sciencemag.org/news/2020/04/united-states-leads-coronavirus-cases-not-pandemic-response. Retrieved 25 April 2020.
- ↑ Luscombe, R. (22 March 2020). "Trump tries to blunt criticism of Covid-19 response as US cases pass 33,000". The Guardian. https://www.theguardian.com/world/2020/mar/22/trump-coronavirus-response-criticism-us-cases. Retrieved 25 April 2020.
- ↑ Perry, M.; Kelland, K.; Nebehay, S. et al. (14 April 2020). "Factbox: Global Reaction to Trump Withdrawing WHO Funding". Reuters. https://www.reuters.com/article/us-health-coronavirus-trump-who-reaction/factbox-global-reaction-to-trump-withdrawing-who-funding-idUSKCN21X0CN. Retrieved 25 April 2020.
- ↑ Melton, M.; (3 April 2020). "Criticizing America over COVID-19 Response". Providence. https://providencemag.com/2020/04/criticizing-america-covid-19-response/. Retrieved 25 April 2020.
- ↑ Clay, J. (31 March 2020). "BBC praises Gov. DeWine's leadership during coronavirus pandemic". ABC6 On Your Side. https://abc6onyourside.com/news/local/bbc-praises-gov-dewines-leadership-during-coronavirus-pandemic. Retrieved 25 April 2020.
- ↑ Renbaum, B. (20 March 2020). "Glendening Praises Hogan's Response to COVID-19". Maryland Reporter. https://marylandreporter.com/2020/03/20/glendening-praises-hogans-response-to-covid-19/. Retrieved 20 March 2020.
- ↑ "Glowing coverage of Cuomo also raises difficult questions". Columbia Journalism Review. 27 March 2020. https://www.cjr.org/analysis/andrew-cuomo-coronavirus-covid19-barkan.php. Retrieved 25 April 2020.
- ↑ Rothwell, J.; Van Drie, H. (27 April 2020). "The effect of COVID-19 and disease suppression policies on labor markets: A preliminary analysis of the data". Brookings. The Brookings Institute. https://www.brookings.edu/research/the-effect-of-covid-19-and-disease-suppression-policies-on-labor-markets-a-preliminary-analysis-of-the-data/. Retrieved 28 April 2020.
- ↑ Rosenberg, J.M. (26 April 2020). "A flood of business bankruptcies likely in coming months". Associated Press. https://apnews.com/b9ae754f44d27671ec63d85542c468f8. Retrieved 28 April 2020.
- ↑ Ting, V. (26 April 2020). "Coronavirus: suicide experts warn of pandemic’s impact on mental health, with Hong Kong’s jobless, poor and elderly most at risk". South China Morning Post. https://www.scmp.com/news/hong-kong/health-environment/article/3081582/coronavirus-suicide-experts-warn-pandemics-impact. Retrieved 28 April 2020.
- ↑ Colaianni, A. (22 April 2020). "“For Now, We Wait”: Postponing Cancer Surgery During the Coronavirus Crisis". The New Yorker. https://www.newyorker.com/science/medical-dispatch/for-now-we-wait-postponing-cancer-surgery-during-the-coronavirus-crisis. Retrieved 28 April 2020.
- ↑ Aubrey, A. (22 April 2020). "Which States Are Doing Enough Testing? This Benchmark Helps Settle The Debate". NPR - Health Shots. https://www.npr.org/sections/health-shots/2020/04/22/840526338/is-the-u-s-testing-enough-for-covid-19-as-debate-rages-on-heres-how-to-know. Retrieved 28 April 2020.
- ↑ Morrison, S. (24 April 2020). "Why America’s coronavirus testing problem is still so difficult to solve". Vox - Recode. https://www.vox.com/recode/2020/4/24/21229774/coronavirus-covid-19-testing-social-distancing. Retrieved 28 April 2020.
- ↑ Achenach, J.; Johnson, C.Y. (29 April 2020). "Studies leave question of ‘airborne’ coronavirus transmission unanswered". The Washington Post. https://www.washingtonpost.com/health/2020/04/29/studies-leave-question-airborne-coronavirus-transmission-unanswered/. Retrieved 01 May 2020.
- ↑ Huang, P. (20 March 2020). "How The Novel Coronavirus And The Flu Are Alike ... And Different". NPR: Goats and Soda. https://www.npr.org/sections/goatsandsoda/2020/03/20/815408287/how-the-novel-coronavirus-and-the-flu-are-alike-and-different. Retrieved 01 April 2020.
- ↑ Resnick, B.; Animashaun, C. (18 March 2020). "Why Covid-19 is worse than the flu, in one chart". Vox. https://www.vox.com/science-and-health/2020/3/18/21184992/coronavirus-covid-19-flu-comparison-chart. Retrieved 01 April 2020.
- ↑ Kumar, V. (27 March 2020). "COVID-19 has been compared to the flu. Experts say that's wrong". ABC News. https://abcnews.go.com/Health/covid-19-compared-flu-experts-wrong/story?id=69779116. Retrieved 01 April 2020.
- ↑ National Water and Climate Center. "Median vs. Average to Describe Normal". U.S. Department of Agriculture. https://www.wcc.nrcs.usda.gov/normals/median_average.htm. Retrieved 01 April 2020.
- ↑ Lauer, S.A.; Grantz, K.H.; Bi, Q. et al. (2020). "The Incubation Period of Coronavirus Disease 2019 (COVID-19) From Publicly Reported Confirmed Cases: Estimation and Application". Annals of Internal Medicine. doi:10.7326/M20-0504. PMC PMC7081172. PMID 32150748. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7081172.
- ↑ Pinsker, J. (19 March 2020). "What Do You Tell Someone Who Still Won’t Stay Home?". The Atlantic. https://www.theatlantic.com/family/archive/2020/03/convince-family-take-coronavirus-seriously/608356/. Retrieved 01 April 2020.
- ↑ Keating, S. (17 March 2020). "When The People You Love Can’t Accept That They Need To Stay Home". BuzzFeed News. https://www.buzzfeednews.com/article/shannonkeating/coronavirus-social-distancing-self-isolation-quarantine. Retrieved 01 April 2020.
- ↑ Jackson, A. (31 March 2020). "Police are arresting and fining people for violating social distancing orders". CNN. https://www.cnn.com/2020/03/31/us/violating-coronavirus-orders-trnd/index.html. Retrieved 01 April 2020.
- ↑ WFLA 8 On Your Side Staff (31 March 2020). "Hawaii police arrest visiting Tampa man for violating 14-day quarantine order". WFLA News Channel 8. https://www.wfla.com/community/health/coronavirus/hawaii-police-arrest-visiting-tampa-man-for-violating-14-day-quarantine/. Retrieved 01 April 2020.
- ↑ 57.0 57.1 Mandavilli, A. (31 March 2020). "Infected but Feeling Fine: The Unwitting Coronavirus Spreaders". The New York Times. https://www.nytimes.com/2020/03/31/health/coronavirus-asymptomatic-transmission.html. Retrieved 01 April 2020.
- ↑ 58.0 58.1 Mock, J. (26 March 2020). "Asymptomatic Carriers Are Fueling the COVID-19 Pandemic. Here’s Why You Don’t Have to Feel Sick to Spread the Disease". Discover. https://www.discovermagazine.com/health/asymptomatic-carriers-are-fueling-the-covid-19-pandemic-heres-why-you-dont. Retrieved 01 April 2020.
- ↑ Yuen, K.-S.; Fung, S.-Y.; Chan, C.-P.; Jin, D.-Y. (2020). "SARS-CoV-2 and COVID-19: The most important research questions". Cell & Bioscience 10: 40. doi:10.1186/s13578-020-00404-4. PMC PMC7074995. PMID 32190290. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7074995.
- ↑ Diamond, F. (17 March 2020). "Asymptomatic Carriers of COVID-19 Make It Tough to Target". Infection Control Today. https://www.infectioncontroltoday.com/covid-19/asymptomatic-carriers-covid-19-make-it-tough-target. Retrieved 01 April 2020.
- ↑ Jordan, R. (26 March 2020). "Environmental engineers at Stanford discuss how to identify factors affecting COVID-19 transmission". Stanford News. https://news.stanford.edu/2020/03/26/understanding-spread-covid-19/. Retrieved 01 April 2020.
- ↑ 62.0 62.1 62.2 Greenfieldboyce, N. (28 March 2020). "WHO Reviews 'Current' Evidence On Coronavirus Transmission Through Air". NPR. https://www.npr.org/2020/03/28/823292062/who-reviews-available-evidence-on-coronavirus-transmission-through-air. Retrieved 01 April 2020.
- ↑ Chicago Sun Times Editorial Board (31 March 2020). "Ignore the mixed messages and wear that mask". Chicago Sun Times. https://chicago.suntimes.com/2020/3/31/21200144/coronavirus-covid-19-masks-wear-cdc-pritzker-trump-public-health-virus-face-cough-sneeze. Retrieved 01 April 2020.
- ↑ Mulholland, J. (29 March 2020). "To mask or not to mask: mixed messages in a time of crisis". RFI. http://www.rfi.fr/en/international/20200329-to-mask-or-not-to-mask-mixed-messages-in-a-time-of-coronavirus-crisis-france-covid-19-spread-droplets. Retrieved 01 April 2020.
- ↑ 65.0 65.1 65.2 65.3 Geddes, L. (27 March 2020). "Does a high viral load or infectious dose make covid-19 worse?". New Scientist. https://www.newscientist.com/article/2238819-does-a-high-viral-load-or-infectious-dose-make-covid-19-worse/. Retrieved 01 April 2020.
- ↑ Hijano, D.R.; Brazelton de Cardenas, J.; Maron, G. et al. (2019). "Clinical correlation of influenza and respiratory syncytial virus load measured by digital PCR". PLoS One 14 (9): e0220908. doi:10.1371/journal.pone.0220908. PMC PMC6720028. PMID 31479459. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6720028.
- ↑ Liu, Y.; Yan, L.-M.; Wan, L. et al. (2020). "Viral dynamics in mild and severe cases of COVID-19". The Lancet Infectious Diseases. doi:10.1016/S1473-3099(20)30232-2. PMID 32199493.
- ↑ Joynt, G.M.; Wu, W.K.K. (2020). "Understanding COVID-19: what does viral RNA load really mean?". The Lancet Infectious Diseases. doi:10.1016/S1473-3099(20)30237-1.
- ↑ 69.0 69.1 Madjid, M.; Safavi-Naeini, P.; Solomon, S.D. (2020). "Potential Effects of Coronaviruses on the Cardiovascular System". JAMA Cardiology. doi:10.1001/jamacardio.2020.1286. PMID 32219363.
- ↑ 70.0 70.1 Xiong, T.-Y.; Redwood, S.; Prendergast, B.; Chen, M. (2020). "Coronaviruses and the cardiovascular system: acute and long-term implications". European Heart Journal: ehaa231. doi:10.1093/eurheartj/ehaa231. PMID 32186331.
- ↑ Driggin, E.; Madhavan, M.V.; Bikdeli, B. et al. (2020). "Cardiovascular Considerations for Patients, Health Care Workers, and Health Systems During the Coronavirus Disease 2019 (COVID-19) Pandemic". Journal of the American College of Cardiology. doi:10.1016/j.jacc.2020.03.031. PMID 32201335.
- ↑ 72.0 72.1 Otto, M.A. (26 March 2020). "Cardiac symptoms can be first sign of COVID-19". The Hospitalist. https://www.the-hospitalist.org/hospitalist/article/219645/coronavirus-updates/cardiac-symptoms-can-be-first-sign-covid-19. Retrieved 01 April 2020.
- ↑ 73.0 73.1 Clerkin, K.J.; Fried, J.A.; Raikhelkar, J. et al. (2020). "Coronavirus Disease 2019 (COVID-19) and Cardiovascular Disease". Circulation. doi:10.1161/CIRCULATIONAHA.120.046941. PMID 32200663.
- ↑ Mehta, P.; McAuley, D.F.; Brown, M. et al. (2020). "COVID-19: Consider cytokine storm syndromes and immunosuppression". The Lancet 395 (10229): P1033–34. doi:10.1016/S0140-6736(20)30628-0. PMID 32192578.
- ↑ 75.0 75.1 Mandavilli, A. (1 April 2020). "The Coronavirus Patients Betrayed by Their Own Immune Systems". The New York Times. https://www.nytimes.com/2020/04/01/health/coronavirus-cytokine-storm-immune-system.html. Retrieved 01 April 2020.
- ↑ Tisoncik, J.R.; Korth, M.J.; Simmons, C.P. et al. (2012). "Into the eye of the cytokine storm". Microbiology and Molecular Biology Reviews 76 (1): 16–32. doi:10.1128/MMBR.05015-11. PMC PMC3294426. PMID 22390970. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3294426.
- ↑ Basilio, P. (26 March 2020). "A new potential risk of COVID-19: Sudden cardiac death". MDLinx. https://www.mdlinx.com/internal-medicine/article/6590. Retrieved 01 April 2020.
- ↑ Rettner, R. (23 April 2020). "Mysterious blood clots in COVID-19 patients have doctors alarmed". LiveScience. https://www.livescience.com/coronavirus-blood-clots.html. Retrieved 28 April 2020.










