Difference between revisions of "Journal:Experimental application of business process management technology to manage clinical pathways: A pediatric kidney transplantation follow-up case"
Shawndouglas (talk | contribs) (Saving and adding more.) |
Shawndouglas (talk | contribs) (Saving and adding more.) |
||
| Line 152: | Line 152: | ||
During six months while the experimental phase was active, we monitored with a stopwatch the time required to complete every activity for each patient under both types of management, which we named “Current Management” and “BPM Management.” | During six months while the experimental phase was active, we monitored with a stopwatch the time required to complete every activity for each patient under both types of management, which we named “Current Management” and “BPM Management.” | ||
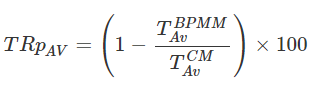
To obtain the average time-reduction percent we used the average time spent per patient with BPM management and the average time spent per patient with current management. These two values represent the average total time spent per patient to manage the clinical pathway, including the retrieval of laboratory results, planning next admissions, and communicating the planning to the stakeholders within the department. The average time | To obtain the average time-reduction percent we used the average time spent per patient with BPM management and the average time spent per patient with current management. These two values represent the average total time spent per patient to manage the clinical pathway, including the retrieval of laboratory results, planning next admissions, and communicating the planning to the stakeholders within the department. The average time reduction percentage estimates the average time saved by the users in the daily clinical pathways management tasks. | ||
[[File:Math1 Andellini BMCMedInfoDecMak2017 17-1.png|313px]] | [[File:Math1 Andellini BMCMedInfoDecMak2017 17-1.png|313px]] | ||
| Line 158: | Line 158: | ||
with TAvBPMM being the average time per patient with BPM management, and TAvCM being the average time per patient with current management. | with TAvBPMM being the average time per patient with BPM management, and TAvCM being the average time per patient with current management. | ||
==Results== | |||
===Time reduction evaluation=== | |||
As mentioned above, in this study we have monitored the activities of the main stakeholder, the transplant coordinator, for six months. During this period, using a stopwatch the coordinator recorded the time spent doing management tasks for 30 effective days. | |||
In order to compare results between the two managing methods, 22 patients were selected to have their clinical pathway managed with the new application. The remaining patients were managed with the current methods. | |||
Figure 3 shows the statistical results obtained during the monitoring period and which were used to calculate the two average values required in the previously mentioned equation to determine the average time-reduction percentage. The total number of values recorded was 173. Eighty (80) time measurements were recorded for use with the BPM application, while 93 were recorded for traditional management. Each point in Fig. 3 represents a time-measurement for the management of the follow-up of a single patient. Some points in the figure may overlap with others. | |||
[[File:Fig3 Andellini BMCMedInfoDecMak2017 17-1.gif|567px]] | |||
{{clear}} | |||
{| | |||
| STYLE="vertical-align:top;"| | |||
{| border="0" cellpadding="5" cellspacing="0" width="567px" | |||
|- | |||
| style="background-color:white; padding-left:10px; padding-right:10px;"| <blockquote>'''Fig. 3''' The statistical results obtained during the monitoring period to estimate the average time-reduction percentage for both methods: current management and the BPM method. The total number of values recorded was 173. Eighty time measurements were recorded for using the BPM application, while 93 were recorded for traditional management. Each point represents a time-measurement for the management of the follow up of a single patient. Each cross represents one measurement of the total time spent for the management of a single patient’s follow-up performed with the traditional method. Each filled triangle represents one measurement of the total time spent for the management of a single patient’s follow-up performed with the BPM method.</blockquote> | |||
|- | |||
|} | |||
|} | |||
Figure 4 shows the average time reduction comparing the different times for the two methods. The percentage of time saved by using the new method is 57.9% (''p'' < 0.001), the average time for the BPM method is four minutes, while the coordinator needs 9.5 minutes with the traditional method (lab time reduction is equal to 37.5%, ''p'' < 0.001; com time reduction is equal to 100%, as the task is no longer performed; plan time reduction is equal to 70.0%, ''p'' < 0.001). | |||
[[File:Fig4 Andellini BMCMedInfoDecMak2017 17-1.gif|472px]] | |||
{{clear}} | |||
{| | |||
| STYLE="vertical-align:top;"| | |||
{| border="0" cellpadding="5" cellspacing="0" width="472px" | |||
|- | |||
| style="background-color:white; padding-left:10px; padding-right:10px;"| <blockquote>'''Fig. 4''' The average time reduction comparing the different times for the two methods. The percentage of time saved by using the new method is 57.9% (''p''<0.001), the average time for the BPM method is four minutes, while the coordinator needs 9.5 minutes with the traditional method (lab time reduction is equal to 37.5%, ''p''<0.001; com time reduction is equal to 100%, as the task is no longer performed; plan time reduction is equal to 70.0%, ''p''<0.001).</blockquote> | |||
|- | |||
|} | |||
|} | |||
Revision as of 00:26, 14 November 2017
| Full article title | Experimental application of business process management technology to manage clinical pathways: A pediatric kidney transplantation follow-up case |
|---|---|
| Journal | BMC Medical Informatics and Decision Making |
| Author(s) | Andellini, Martina; Riesgo, Sandra Fernandez; Morolli, Federica; Ritrovato, Matteo; Cosoli, Piero; Petruzzellis, Silverio; Rosso, Nicola |
| Author affiliation(s) | Bambino Gesù Children’s Hospital, Openwork Srl |
| Primary contact | Email: martina dot andellini at opbg dot net |
| Year published | 2017 |
| Volume and issue | 17 (1) |
| Page(s) | 151 |
| DOI | 10.1186/s12911-017-0546-x |
| ISSN | 1472-6947 |
| Distribution license | Creative Commons Attribution 4.0 International |
| Website | https://bmcmedinformdecismak.biomedcentral.com/articles/10.1186/s12911-017-0546-x |
| Download | https://bmcmedinformdecismak.biomedcentral.com/track/pdf/10.1186/s12911-017-0546-x (PDF) |
|
|
This article should not be considered complete until this message box has been removed. This is a work in progress. |
Abstract
Background: To test the application of business process management (BPM) technology to manage clinical pathways, using a pediatric kidney transplantation as case study, and to identify the benefits obtained from using this technology.
Methods: Using a business process management platform, we implemented a specific application to manage the clinical pathway of pediatric patients, and we monitored the activities of the coordinator in charge of case management during a six-month period (from June 2015 to November 2015) using two methodologies: the traditional procedure and the one under study.
Results: The application helped physicians and nurses to optimize the amount of time and resources devoted to management purposes. In particular, time reduction was close to 60%. In addition, the reduction of data duplication, the integration of event management, and the efficient collection of data improved the quality of the service.
Conclusions: The use of business process management technology, usually related to well-defined processes with high management costs, is an established procedure in multiple environments; its use in healthcare, however, is innovative. The use of already accepted clinical pathways is known to improve outcomes. The combination of these two techniques, well established in their respective areas of application, could represent a revolution in clinical pathway management. The study has demonstrated that the use of this technology in a clinical environment, using a proper architecture, and identifying a well-defined process leads to real benefits in terms of resource optimization and quality improvement.
Keywords: clinical pathway, kidney transplantation, pediatrics, case management, business process management
Background
During recent years, two of the most important goals in healthcare have been the optimization of resources and the improvement of efficiency and quality.
These objectives have become vital in view of the limited ability of health organizations to adopt information technology (IT) due to the complexity of these organizations and their fragmented internal structures. In other words, healthcare institutions have been managed individually using ad hoc solutions. The critical elements in healthcare management are variability due to different availability of healthcare services, scarce use of medical evidence, and the phenomena of professional uncertainty. This has led to a slow evolution in healthcare management and optimization because new methodologies, technologies, and practices have not been implemented in healthcare environments at the same rate as in other sectors.[1] This aspect is critical because the main objective of health care services is to reduce cost without reducing the quality of patient care. To reach the best cost-quality ratio, healthcare management has to reach the same level as other services in terms of efficiency; to do this we will need to follow the same path as other sectors, not hesitating to implement new and available technologies and methodologies.
One such methodology developed in and established internationally since the 1980s is the implementation of clinical pathways to guide evidence-based healthcare.[2] Clinical pathways are clinical management tools used to manage the quality of health care through the standardization of care processes. Clinical pathways are an evidence-based response to specific health care problems and provide physicians and nurses with a pre-established care plan, devised according to international standards and developed by specialists in the field. The application of these standards helps professionals offer patients the best possible care plan, without needing to devise an individual care plan for each patient, thus avoiding human error and saving time for both physicians and patients.[3]
The management of these care plans is often a complex task, as the pathway integrates several guidelines, with different tests that have to be performed at specific time points. A clinical pathway timeline defines the expected plan of treatments for a group of patients with a particular diagnosis or undergoing a particular clinical procedure. It outlines a time-specified plan of treatment, recommending tests and therapies based upon a combination of clinical practice consensus and evidence from the scientific literature, thus leading to an improvement in the quality of clinical outcomes.[3] When the pathway is applied to a large set of patients, management becomes a time-consuming activity. It has been shown that their implementation reduces the variability in clinical practice and improves clinical outcomes.[3]
All the tests planned for the pathway must be coordinated according to the resources available and to the pathway schedule, including the specific variations according to the clinical situation of the patient.
Adverse events are another parameter to be included in case management. When a patient experiences an adverse event, specific guidelines or protocols are followed.
With the above premises, we hypothesized that using business process management (BPM) techniques would improve the coordination task. BPM is a discipline that has evolved since the 1990s and has been adopted in many environments to manage and optimize end-to-end processes. In healthcare, these techniques have only been used during the last two decades[4] since they provide support at the business or organization level and are usually applied to well-defined processes. In the clinical environment, the integration of this tool is innovative. A literature search, limited to PubMed, found very few articles (four) using the terms “pathways” and “business process management,” and none of them described a practical implementation.
Methods
The aims of this work were to define a clinical pathway as a process, using a pediatric kidney transplantation as a case study, and to identify the benefits obtained from using this technology by monitoring particular characteristics and many parameters. We sought to have a wider view of the complex clinical process and to manage each patient case efficiently, integrating events and variations for each individual situation. We believed that achieving this aim would lead to an increase in the quality of the work carried out by healthcare workers and a decrease in workload.
We have not limited our project to abstractions; it also includes concrete and practical aspects. We have developed a web-based application to integrate the BPM approach in the management of clinical pathways.
The context
The standard business process modeling notation (BPMN) has been already used at Bambino Gesù Children’s Hospital (Rome, Italy) for a previous project, whose objective was the optimization and planning of operating theatre activities.[5] Bambino Gesù Children’s Hospital is the largest Italian pediatric hospital managing high-complexity cases of kidney transplantation. In the hospital, transplants are performed in children with more than eight kilograms body weight. All aspects of childcare are taken into account through an integrated and multidisciplinary approach, including psychological development.[6]
During each patient admission, either in the day hospital or in the ward, a member of the transplant team has to:
- search the patient data in the hospital repository (personal data, medical reports, laboratory analysis results and follow-up plan)
- select only clinical data relevant for decision-making, assisted by creating for instance special filters on the results
- save the data in a shared document in specific folders of the file system, following an internal coding standard for classifying information
This means that for each patient at each visit, the transplant coordinator has to check which exams have already been performed and what is still to be done, and create a specific program for each patient. A patient may miss an appointment for several reasons and, in this case, another appointment has to be planned and patient lists need to be rearranged. Moreover, results are currently stored in a database which does not allow direct downloading from the hospital system.
To monitor the entire pathway of a single patient, the clinical team needs to navigate the clinical repository to access all the relevant data and copy them into a shared folder, including the specific documents for kidney transplantation.
Coping with the variability of the process is therefore a matter of considerable manual file manipulation, with a difficult-to-manage and error-prone information sharing practice. Currently we have a list of tests (laboratory, instrumental, specialist visits) that must be performed every year at a specific time point according to international guidelines[7][8][9][10][11][12][13] Feeding the database is thus a time-consuming task for the transplant coordinator.
Having a computerized system with a specifically designed database, which interacts with the hospital clinical repository, should allow the prompt retrieval of patient data. This will be of great help in guiding clinical decisions and in carrying out research projects. In addition, scheduling patients’ appointments could be automatic, reducing human mistakes and leading to time saving.
As a result, this process was selected for the experimental application of BPM technology to prove the feasibility of its implementation and identify the benefits deriving from its use.
Several techniques and practices based on new technology and innovative patterns and approaches have been used during recent years in an attempt to attain the optimization goal. One of these is the above-mentioned business process management (BPM).
BPM is a discipline designed to improve processes and help organizations to manage their activities efficiently. It involves any combination of modeling, automation, execution, control, measurement, and optimization of flows, as stated in the definition given by Nathaniel Palmer[14], VP and CTO of BPM, Inc.
BPM is intended for analysis and design and uses a specific notation recognized as an international standard: Business Process Modeling Notation (BPMN 2.0). We used the latest version, BPMN 2.0 for the analysis and design phases of the project.[15]
Approach
Once a pathway had been identified, interviews and meetings were held to share knowledge of the case with the IT team, whose first responsibility was the analysis of the case and the process definition. To complete the global analysis of the case, more interviews were held to elicit the requirements of the physicians and nurses of the coordination center. Once all the information necessary for the application had been obtained, the team was able to produce a document defining the process that would be managed automatically by the application and meet the requirements of the final users.
The next task was to translate all the information and requirements into a design document, directed towards the implementation of the application using the Jamio platform; for the process definition, we used the BPMN 2.0 standard.[15]
The design document was used as input for the implementation of the application. The Jamio platform offers a BPM editor, called Composer, which uses BPMN 2.0 to create processes. This tool allows the user to reproduce the whole domain: the different kinds of users, the data types, the relationships, the rules, the layout, etc.
After the first version of the implementation, iterations were discussed with the final users, with the aim to improve the satisfaction level and to offer the users the opportunity to become familiar with the tool.
When the final version was delivered, the team organized a presentation with the technological partners and medical teams to share the results of all the work done.
Several iterations suggested by the users have been implemented since then.
Technology
To develop the application, we have used the Jamio Platform (Openwork Srl), which integrates BPMN 2.0 into its modeling tool for design and implementation.[15]
The system was selected to meet key requirements of both the user panel and the IT department:
- the possibility for clinicians to design the standard basic protocol without the involvement of IT people
- the possibility to cope with unexpected events occurring during care path activities
- the possibility to access and integrate clinical repository data during follow-up activities
- the possibility to involve different stakeholders, belonging to different organizations or institutions
- the possibility to analyze clinical data collected during the entire course of the care path
- the possibility to monitor and analyze the cost of activities during follow-up
The system was implemented using a BPM-based platform with a service-oriented architecture (SOA) to facilitate access to the clinical repository using web services. Moreover, the platform provided integrated human task management capabilities and was able to orchestrate services with an event-based approach. The platform’s model-driven approach allowed the detailed specification of protocols by clinicians and the integrated recording of the scheduled activities by the appointed stakeholders. This enabled the system to embrace and manage both planned actions and unexpected events diverging from the protocols predefined by clinicians.
The whole set of activities, both those planned in advance and those resulting from an unexpected event that could influence follow-up, can be assigned to the appropriate actors according to the activity to be performed, thanks to the capacity of the integrated organization management services to map virtually the organization of the departments involved in the case.
The BPM-based platform supports the follow-up process design completely, involving both the clinicians and the IT department, allowing them to manage their respective domains with the appropriate instruments.
Process analysis
This study is an example of case management implementation, so the first task was to assemble all available knowledge concerning the case. The starting point for this purpose was the standard monitoring protocol applied to each patient. Based on the stakeholders’ knowledge and the documents provided, we have created a process to represent the clinical pathway. Figure 1 shows the first part of the clinical protocol foreseen for the first year after transplantation. Each group of tests to be performed is planned for a specific period, their frequency varying throughout the process. Figure 2 shows the cyclical process to be followed after completing the first-year protocol. The combination of the two figures shows the entire clinical pathway applied to the patients, which is the final process to be managed by the BPM application. These two activity diagrams were the main output of the process definition phase.
|
|
Although these diagrams show a well-defined monitoring plan, in real life most of the protocols are modified according to the clinical situation of each patient. This means that the main requirement is flexibility and possibility to customize on a per-patient basis each process at run time after the automatic creation of the “template care plan.” The case shown is quite complex from this point-of-view due to the fact that an event may occur at any moment and the consequences are only known when the clinical team makes a decision on how to manage them.
The necessity of having a flexible process was the main reason for adopting the innovative architecture. Usually, when using BPM, the process is well defined and static, but this is not the case. For these reasons, we defined a proper architecture and identified a well-defined process to improve the flexibility that fit our need. The process that manages the pathway, instead of being a complex single process, is divided into three main managing processes.
- The first one receives the medical visit templates introduced by the administrator and generates the default pathway for the patient.
- The second process runs daily and creates the human tasks and visit templates whose dates are included in the planning period.
- The third one manages the actions to perform when the user creates a new patient event in the platform solution.
Evaluation methods
For this initial evaluation, time reduction was selected as the main parameter for evaluating the application introduction.
In order to evaluate the time reduction, the experiment proposed was to manage with the new application a set of 22 patients, selected from among all the patients. By monitoring the daily activity of the coordinator for the two groups, i.e., the 22 patients managed with the application and the rest (248) with the traditional method, we were able to compare the time taken to manage the integrated clinical pathway for each patient in the two groups.
During six months while the experimental phase was active, we monitored with a stopwatch the time required to complete every activity for each patient under both types of management, which we named “Current Management” and “BPM Management.”
To obtain the average time-reduction percent we used the average time spent per patient with BPM management and the average time spent per patient with current management. These two values represent the average total time spent per patient to manage the clinical pathway, including the retrieval of laboratory results, planning next admissions, and communicating the planning to the stakeholders within the department. The average time reduction percentage estimates the average time saved by the users in the daily clinical pathways management tasks.
with TAvBPMM being the average time per patient with BPM management, and TAvCM being the average time per patient with current management.
Results
Time reduction evaluation
As mentioned above, in this study we have monitored the activities of the main stakeholder, the transplant coordinator, for six months. During this period, using a stopwatch the coordinator recorded the time spent doing management tasks for 30 effective days.
In order to compare results between the two managing methods, 22 patients were selected to have their clinical pathway managed with the new application. The remaining patients were managed with the current methods.
Figure 3 shows the statistical results obtained during the monitoring period and which were used to calculate the two average values required in the previously mentioned equation to determine the average time-reduction percentage. The total number of values recorded was 173. Eighty (80) time measurements were recorded for use with the BPM application, while 93 were recorded for traditional management. Each point in Fig. 3 represents a time-measurement for the management of the follow-up of a single patient. Some points in the figure may overlap with others.
|
Figure 4 shows the average time reduction comparing the different times for the two methods. The percentage of time saved by using the new method is 57.9% (p < 0.001), the average time for the BPM method is four minutes, while the coordinator needs 9.5 minutes with the traditional method (lab time reduction is equal to 37.5%, p < 0.001; com time reduction is equal to 100%, as the task is no longer performed; plan time reduction is equal to 70.0%, p < 0.001).
|
References
- ↑ England, I.; Stewart, D.; Walkers, S. (2000). "Information technology adoption in health care: When organisations and technology collide". Australian Health Review 23 (3): 176–85. doi:10.1071/AH000176. PMID 11186051.
- ↑ Kinsman, L.; Rotter, T.; James, E. et al. (2010). "What is a clinical pathway? Development of a definition to inform the debate". BMC Medicine 8: 31. doi:10.1186/1741-7015-8-31. PMC PMC2893088. PMID 20507550. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2893088.
- ↑ 3.0 3.1 3.2 Panella, M.; Marchisio, S.; Di Stanislao, F. (2003). "Reducing clinical variations with clinical pathways: Do pathways work?". International Journal for Quality in Health Care 15 (6): 509-21. doi:10.1093/intqhc/mzg057. PMID 14660534.
- ↑ González Sánchez, M.J.; Framiñán Torres, J.M.; Parra Calderón, C.L. et al. (2008). Andersen, S.K.; Klein, G.O.; Schulz, S. et al.. ed. Application of business process management to drive the deployment of a speech recognition system in a healthcare organization. Studies in Health Technology and Informatics. 136. pp. 511–16. ISBN 9781607503330.
- ↑ Barbagallo, S.; Corradi, L.; de Ville de Goyet, J. et al. (2015). "Optimization and planning of operating theatre activities: An original definition of pathways and process modeling". BMC Medical Informatics and Decision Making 15 (1): 38. doi:10.1186/s12911-015-0161-7. PMC PMC4436841. PMID 25982033. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4436841.
- ↑ Tozzi, A.E.; Mazzotti, E.; Di Ciommo, V.M. et al. (2012). "Quality of life in a cohort of patients diagnosed with renal failure in childhood and who received renal transplant". Pediatric Transplantation 16 (8): 840–5. doi:10.1111/j.1399-3046.2012.01774.x. PMID 22943602.
- ↑ Cohen, D.; Galbraith, C. (2001). "General health management and long-term care of the renal transplant recipient". American Journal of Kidney Diseases 38 (6 Suppl. 6): S10–24. doi:10.1053/ajkd.2001.28922. PMID 11729002.
- ↑ Adams, P.L. (2006). "Long-term patient survival: strategies to improve overall health". American Journal of Kidney Diseases 47 (4 Suppl. 2): S65–85. doi:10.1053/j.ajkd.2005.12.043. PMID 16567242.
- ↑ Howard, A.D. (2006). "Long-term posttransplantation care: The expanding role of community nephrologists". American Journal of Kidney Diseases 47 (4 Suppl. 2): S111–24. doi:10.1053/j.ajkd.2005.12.040. PMID 16567237.
- ↑ Josephson, M.A. (2011). "Monitoring and managing graft health in the kidney transplant recipient". Clinical Journal of the American Society of Nephrology 6 (7): 1774-80. doi:10.2215/CJN.01230211. PMID 21734093.
- ↑ Hariharan, S. (2006). "Recommendations for outpatient monitoring of kidney transplant recipients". American Journal of Kidney Diseases 47 (4 Suppl. 2): S22–36. doi:10.1053/j.ajkd.2005.12.046. PMID 16567238.
- ↑ Kasiske, B.L.; Vazquez, M.A.; Harmon, W.E. et al. (2000). "Recommendations for the outpatient surveillance of renal transplant recipients". Journal of the American Society of Nephrology 11 (Suppl. 1): S1–86. PMID 11044969.
- ↑ Howard, A.D. (2001). "Long-term management of the renal transplant recipient: Optimizing the relationship between the transplant center and the community nephrologist". American Journal of Kidney Diseases 38 (6 Suppl. 6): S51–7. doi:10.1053/ajkd.2001.28926. PMID 11729006.
- ↑ Palmer, N. (26 March 2014). "What Is BPM?". BPM.com. Business Process Management, Inc. https://bpm.com/what-is-bpm. Retrieved 04 February 2016.
- ↑ 15.0 15.1 15.2 "Business Process Model and Notation (BPMN) Version 2.0" (PDF). Object Management Group. January 2011. http://www.omg.org/spec/BPMN/2.0/PDF/. Retrieved 04 February 2016.
Notes
This presentation is faithful to the original, with only a few minor changes to presentation. In several cases the PubMed ID was missing and was added to make the reference more useful. Grammar and vocabulary were cleaned up to make the article easier to read. The original duplicated citation three and four; they have been combined into one citation (three) for this version.